Biological causality for T4 monotherapy not working for some is now established. We can’t now attribute the 10%–15% of people with hypothyroidism not feeling better on T4 as wimps, laggards, or requiring psychological attention. Sarah Cathcart Evans reflects from personal experience of
Though it is widely known that kidney donation is common among living donors who are family or friends, there appears to be lower awareness of kidney donation along a non-directed pathway. Here, Rich Armitage describes the process of becoming a non-directed altruistic
Peter McNelly provides an introduction to the role of the mental health practitioner in general practice, and how they can help reduce the workload of GPs.
Some patients with medically unexplained symptoms (MUS) suffer years of referrals and inconclusive tests. Others find themselves overlooked by health care services and feel forgotten. However, diagnostic delay may be due to a disease being rare. Stephen Walker and colleagues offer a
New research into the serotonin theory of depression raises two separate, but related issues. The first is our understanding about the aetiology of depression. The second is understanding why we prescribe antidepressants. Nada Khan reflects on what this means for general practice.
Richard Armitage looks at the health needs of people who work away from home, be they itinerant telecommuters or contract-workers in haulage and construction - should general practice be evolving to meet the access needs of this group? Join the discussion!
Sharon Dixon and colleagues contend that a deeper understanding of safeguarding practices (and how these look and feel on the front-line of multi-agency encounters) is needed if future child safeguarding tragedies are to be avoided.
Richard Armitage argues that good management of hay fever represents an opportunity for general practice to reduce suffering and restore both wellbeing and economic activity to the nation!
TDR programmes consist of a low calorie (around 800 kcal/day) formula diet alongside a stepped food reintroduction as well as regular behavioural support. Yusuf Ben-Tarifite examines the evidence for TDR in Type 2 Diabetes Mellitus.
The winners are in for the Research Paper of the Year award 2021! Carolyn A Chew-Graham and Helen Leach present the winners and stand outs from this year's awards, with reflection on the importance of primary care research for GP trainees working
In April 2020, NICE published new guidance on how to help patients to safely stop antidepressant use. To help GPs to implement this guidance in their practice, Stevie Lewis from the International Institute for Psychiatric Drug Withdrawal and Mark Horowitz have published
Karen Nicholson highlights possible connections between psychological trauma fibromyalgia and chronic pain syndromes - and suggests an audit
Aaron Poppleton, Dennis Ougrin, and Yana Maksymets give a responsive overview of the health needs of Ukrainian refugees and provide a list of useful resources for GPs
Nada Khan considers how to approach HRT shortages in general practice
Nada Khan discusses practical aspects of supporting migrants from Ukraine in UK primary care.
Drs Laura Heath and Sheena Sharma present their bereavement toolkit, designed to aid healthcare practitioners navigate this potentially difficult space by providing real-world consultation ‘tools’.
Ayesha Siddqui shares a clinical case to remind GPs why it is vital to heed clinical cues and check patient vital signs
Krishnakant Buch's GP exploded a telephonic bomb shell: ‘You have type 2 diabetes'. Here he tells us what he did about it, and how he conquered the Diabetes UK, one million step challenge.
The immune-system is complex and is interconnected with the central nervous and endocrine systems. Regina Ford discusses a wide range of scientific research that looks at diet, supplements, exercise, sleep quality and stress/mental health, to give us a holistic overview of health
Making a diagnosis is like detecting the correct clues to solve a crime. But Samar Razaq reminds us that in general practice the crime scene seems to keep on changing......
Data suggests that the interventions put in place to control the pandemic may have reduced the childhood population’s resistance to normal endemic diseases leading to a ‘build-up of susceptibility’. Roshni Mistry and James Hibberd warn us to be prepared for a possible
The good news is that palliative care is reaching more people with cancer, organ failure and frailty and dementia, and is starting earlier. But Scott Murray and Jordi Amblas question why planned and emergency medical care continues to expand even more for
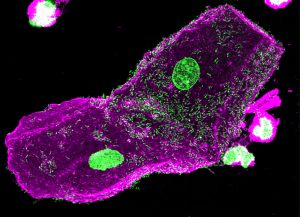
Severe combined immunodeficiency (SCID) affects approximately 14 infants a year in England. The condition is usually fatal by 12-18 months of age without bone marrow transplantation. Public Health England will be performing a two year evaluation of newborn screening for SCID in
The UK Government announced its intention to introduce a national system of medical examiners in England which will result in the scrutiny of all deaths not referred to the coroner. Frances Cranfield explains what we need to know.
From this year GP registrars will be spending two years of their training in the community. Rachel Roberts and her colleagues share their findings from a pilot scheme.
GPDPR is a new initiative from NHS Digital to collect data held in GP medical records, to be available to third parties for research and planning. Unlike most other projects, patients have to actively opt out if they do not want their
Most of those who die by suicide contact primary care in the year or months prior to the suicide. GPs are a trusted and valued source for help-seeking among those who are at-risk of suicide. So how can we help? Maria Michail
Most children removed from their birth family have experienced multiple traumas. Hannah Milton finds that when talking to patients about anxiety, depression, addiction, relationship problems and difficulties with their own children’s behaviour, one her most useful history taking techniques is a simple
Preventing ill health requires an emphasis on the behaviours. Changing patient behaviour can take years and necessitates sustained resources. Vasumathy Sivarajasingam introduces us to the basics of motivational interviewing.
Advance care planning conversations for people likely to be in the last year of life are often not easy. Charles Daniels offers us “the 4 W’s + 1” - a straightforward tool for having difficult advance care planning discussions.
Not many of us expect to be working for the NHS for 50 years. Zarmina Rayaz reports on a remarkable colleague, and tells us what what keeps him going.
The "Defeat Depression" campaign of the 1990s told us that anxiety and depression were caused by a “chemical imbalance in the brain”, and that SSRIs were safe, effective and non-addictive. We now know that virtually every part of that narrative is untrue.
We cannot prevent dying, but we can certainly prevent much unnecessary suffering and overtreatment. Scott Murray shows us how we can incorporate "Anticipatory Care" into the ordinary GP consultation.
After experiencing severe antidepressant withdrawal in 2017, Edward White writes on the failure of healthcare services to recognise symptoms of, and correctly diagnose, antidepressant withdrawal, causing many to turn from primary care to antidepressant withdrawal Facebook groups.
As GPs we know a lot about recurrent urinary tract infections. James Malone-Lee is Emeritus Professor of Medicine, University College London. His research suggests that most of what we think we know is wrong. Here he explains the evidence.
Vasumathy Sivarajasingam describes how we can proactively identify and support victims of domestic abuse.
A crash course in the methodology behind health coaching studies, covering: presense, goal definition, self-awareness, practical application, and the growth mindset. Known to benefit both the consultation process and the clinician, health coaching has the potential to improve outcomes for patient choice
"I ask them - but I'm not asking them in a way that invites a 'yes'" - It can be difficult to broach the subject of self-harm or suicidal thoughts during a consultation. After altering her practice since reading Ford et al's
With the incidence rate of coeliac disease in the UK increasing four-fold between 1990 and 2011, it is essential that patients with coeliac disease continue to receive appropriate support and management during the COVID-19 pandemic. Here, Yvonne Jeanes et al. outline how
With COVID-19 forcing a shift to predominantly remote consulting, how do we ensure that physician associates are fully supported in their role in primary care? The Sheffield Physician Associate (PA) Preceptorship scheme may be one way, offering a formalised support package for
Half of patients with elevated blood sugars, with an HbA1c greater than 42, are not clinically obese. As well as the usual measures Sarah Blake asks whether we need to pay more attention to post prandial blood sugar spikes - is it