At the 44th Annual Conference of the Society for Academic Primary Care I presented results from our study to assess the diagnostic accuracy of self-monitoring blood pressure (BP) for diagnosing hypertension in primary care. Here is a synopsis of that presentation.
High blood pressure is one of the biggest underlying risk factor for cardiovascular disease (CVD) and that CVD itself is the biggest cause of premature death globally. Therefore, accurate diagnosis of high blood pressure is pretty crucial.
Current NICE guidance advocates suspecting hypertension if clinic blood pressure is 140/90 mmHg or greater on 2-3 occasions over a period of weeks to months. If there is a suspicion then the patient should be offered ambulatory blood pressure monitoring which collects the average blood pressure taken over 24 hours using a special electronic monitor that automatically takes measurements 2 to 3 times an hour (1 per hour at night – more than this would be unkind). This is currently considered the “gold” or reference standard for diagnosing high blood pressure. However, not everybody can tolerate this intense level of monitoring. In these cases the guidance advocates home blood pressure monitoring.
Nearly one third to two-thirds of people with suspected high blood pressure already monitor their own blood pressure with an electronic device readily available in their local pharmacy.
But how long should you take home BP measurements to make a diagnosis of hypertension?
Current guidelines for self-monitoring to diagnose high blood pressure state that people should take 2 measurements in the morning and 2 in the evening for 7 days. Doctors should then take an average of all the measurements except those taken on the first day. This is because there is some evidence that self-monitored blood pressure measurements taken on day 1 are often higher than subsequent days due to anxiety or unfamiliarity with the device. The average is then used to determine if someone has high blood pressure or not.
However, the evidence for these recommendations isn’t particularly strong, and no one has assessed what effect these recommendations have on the ability to detect if a person has high blood pressure or not.
Therefore, we conducted a diagnostic accuracy study to find out. This sort of study basically looks at how well a new/alternative test or measurement identifies if a person (usually a patient) does or does not have a particular disease or health condition. Simply put, it’s the way health professionals ask “does the test work?” (it’s actually a little more nuanced than this – anyone interested can follow up here).
Our study set out to look at how current recommendations for self-monitoring impact on its accuracy for diagnosing high blood pressure. We also wanted to look at if using more or less readings from self-monitoring would have an impact on diagnostic accuracy and whether self-monitoring performed in the GP surgery would be better at identifying people with high blood pressure than readings taken by the GP
So what did we do?
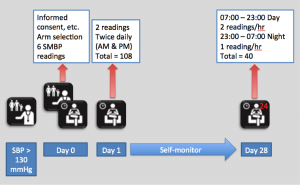
Figure 1 illustrates our study protocol. Patients had their blood pressure measured by their GP (or nurse). They then performed 6 self-monitoring readings in their GP surgery. We then asked patients to self-monitor their blood pressure (according to current guidelines) at home or work for 28 days. This was followed by a 24 hour ambulatory recording.
For each patient, we used the average daytime readings from the 24-hour ambulatory recording to diagnose high blood pressure. We then compared the average blood pressure from self-monitored readings taken over 7 days (discarding day 1 readings as per guideline recommendations).
So what did we find?
As expected, compared with measures taken by a doctor (or nurse) in a GP surgery, the average of 7 days readings taken by patients at home (or work) using an electronic monitor was more accurate at identifying whether someone had high blood pressure or not (see Figure 2).
Figure 2. Sensitivity = for every 100 patients, the values in this row represent the number of patients who actually have hypertension that will be correctly identified by each test (e.g. first column = 95 out of 100 patients who have hypertension will be correctly identified as having hypertension when GPs take the readings). Specificity = for every 100 patients, the values represent the number of patients who do not have hypertension that will be correctly identified by each test (e.g. only 7 out of 100 patients who do not have hypertension will be correctly identified as not having hypertension by the GP).
OK, so not exactly a groundbreaking finding there then. However, when we looked at whether adding more or less readings affected the accuracy of self monitoring (we expected an improvement), we found that the best accuracy came from the first 5 days of self-monitoring.
Increasing the number of readings beyond day 5 (i.e. 20 readings) had surprisingly little effect on the ability to correctly identify high blood pressure or not. The was due to the fact that self-monitoring readings produced on average a higher (around 7 mm Hg) blood pressure when compared with 24 ambulatory monitoring.
Finally, we found that including self-monitored readings taken on day 1 to calculate the average blood pressure had no effect on the ability to detect high blood pressure or not (see Figure 3).
Figure 3.
Our study showed that home monitoring is best used as a test to rule out hypertension (for those interested, the techy bits about how we determined this can be found here) and that doctors can just as accurately identify patients without hypertension from 5 days of self-monitoring. There’s also no need to worry about excluding readings taken on the first day.
So what does this mean in clinical practice?
One of the GP practices involved in our study has adopted this new regime for diagnosing hypertension and has noted significantly shorter waiting times for home-monitoring assessments and quicker diagnostic decisions. We anticipate that our findings and impact cases will be used to underpin updates of current NICE Hypertension guidelines.
Reference
Declaration of interest
This project was part of an independent research project commissioned by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research funding scheme (RP-PG-0407–10347). The views expressed in here are those of the author and not necessarily of the NHS, the NIHR or the Department of Health.
Anyone wanting but unable to access our paper please email me for a copy at david.nunan@phc.ox.ac.uk