 Nada Khan is an Exeter-based NIHR Academic Clinical Fellow in general practice and GPST4/registrar, and an Associate Editor at the BJGP. She is on Twitter: @nadafkhan
Nada Khan is an Exeter-based NIHR Academic Clinical Fellow in general practice and GPST4/registrar, and an Associate Editor at the BJGP. She is on Twitter: @nadafkhan
I recently described the different ‘shelves’ contributing to the GP workforce in response to Charlie Massey’s assertion that there is no shelf with spare GPs, ready and waiting to be plucked into action.1 There are two shelves I neglected to mention, that is, the shelf with locum GPs, and the shelf of academic GPs. What is the contribution to the GP workforce of these shelves of GPs, and how might they impact on workforce pressures in the UK?
Locum GPs
Locum GPs are an essential part of the GP workforce, often covering gaps at short notice and planned absences such as maternity leave or study leave. Why locum? No one GP will have the same reason, but locum GPs report that having more control over how, where and when they work helps prevent burnout in an overstressed healthcare system.2 Aggregate locum GP use in England has been relatively stable from 2017 to 2020, making up around 3% of total GP full-time equivalence (FTE) workforce.3 Locum GPs have been accounting for a greater share in the GP workforce as the overall numbers of GP partners and salaried GPs has fallen since 2017.4 Most locums (74%) are in long-term positions, and in terms of the composition of the workforce, locums are relatively young (median age 42 years), and a small majority are UK graduates (64%).3 Locum use is not uniform across the UK, and a recent analysis in the BJGP looking at locum use in England includes a hot and cold map demonstrating a wide geographical variation in locum use.3 Areas such as the north west of England and London, along with rural practices, had relatively high locum use, with up to 7.4% of the total GP FTE covered by locum GPs.
Locum GPs are an essential part of the GP workforce, often covering gaps at short notice and planned absences such as maternity leave or study leave.
These analyses of locum rates use NHS digital data, which differentiates them between ‘regular’ locums with consistent and predicable working patterns and a planned and ongoing presence in the workforce, versus ‘ad-hoc’ locums who work briefly at a practice to cover short-term or unexpected absences. These ‘ad-hoc’ locums (please note, this is NHS digital’s nomenclature and not mine) sometimes hold other roles within the workforce. Interestingly, in their descriptions, NHS digital suggest that ad-hoc locums don’t provide an additional resource for the NHS as they are essentially a ‘cover’ for absences in the workforce, not an extra pair of hands.5
The GP locum workforce is complex, and it is difficult to get an actual headcount of the workforce as some GPs work solely as locums, working a varying number of sessions, while others hold other roles within the GP workforce. My take is that it’s probably not as important to know the exact (and likely changeable number) of GPs who locum, but it might be interesting to see patterns amongst certain groups. How many newly qualified GPs move straight into locuming without taking a salaried position, and how long before (if ever) they take on a salaried post? And what has been the impact on locuming rates of the New to Practice Fellowship, which is only offered to newly qualified GPs who take on a substantive post?
The UK government is not keen on a locum workforce, which they describe as a symptom of the recruitment and retention crisis in general practice. The Health and Social Care committee asserts that nobody should be ‘forced’ (again, their words and not mine) to work as a locum to ‘regain control over their working life’, and suggests that practices could encourage locum GPs back into regular employment by offering more flexible working patterns.6 Flexible working is not the only reason why GPs locum, and if we really treat locuming as a symptom of an overburdened NHS, then we need to reflect on the deeper challenges facing general practice and the NHS and the reasons why GPs choose to locum.
…if we really treat locuming as a symptom of an overburdened NHS, then we need to reflect on the deeper challenges facing general practice and the NHS and the reasons why GPs choose to locum.
The Academic GPs shelf
GPs clinical academics include those who support and develop teaching of undergraduate and postgraduate general practice teaching, and those who work in a research role often affiliated with a university. The Medical Schools Council estimates that there are 260 FTE senior academic GPs in the UK.7 Although some funded academic roles have set percentages of clinical time, not every academic GP works in this way, and it’s unclear what the FTE of academic GPs is in proportion to the overall workforce. Some academic GPs have dual personalities as partners, salaried GPs, or locums, so it’s also unclear what other shelves they may sit on alongside their university roles.
A wide range of backgrounds and GPs ready to contribute to the workforce
Charlie Massey’s assertion that there are no spare GPs has led him to propose the use of specialty and associate speciality (SAS) doctors as a solution to the workforce crisis. In a sense, however, locum GPs are exactly that, a cadre of GPs ready to be plucked into work, though many practices still report difficulties in getting locum cover when it is needed.8 Although the locum workforce has remained relatively stable, the Health and Social Care committee criticises their use as expensive, inequitable and negatively impacting on continuity, and wants to see a move away from a reliance on locum GPs in practice. The locum workforce has been described as a ‘symptom’ of the recruitment and retention crisis in primary care, which may be misleading if we fail to count the variety of reasons why a doctor chooses to locum. However, if we can better understand the locum workforce, and tease out the intricacies of who locums, how many GPs solely locum and why and at what stage of their career, we might be closer to understanding retention and some of the difficulties in recruiting GPs to substantive posts.
References
- In full: Charlie Massey’s speech on SAS doctors: Pulse 2023 [Available from: https://www.pulsetoday.co.uk/special/workforce/in-full-charlie-masseys-speech-on-sas-doctors/.
- Hall LH, Johnson J, Heyhoe J, Watt I, Anderson K, O’Connor DB. Strategies to improve general practitioner well-being: findings from a focus group study. Fam Pract. 2018;35(4):511-6.
- Grigoroglou C, Walshe K, Kontopantelis E, Ferguson J, Stringer G, Ashcroft DM, et al. Locum doctor use in English general practice: analysis of routinely collected workforce data 2017-2020. Br J Gen Pract. 2022;72(715):e108-e17.
- Shembavnekar NB, J.; Bazeer, N.; Kelly, E.; Beech, J.; Charlesworth, A.; McConkey, R.; Fisher, R. Projections: General practice workforce in England: The Health Foundation; 2022 [Available from: https://www.health.org.uk/publications/reports/projections-general-practice-workforce-in-england
- General Practice Workforce, 31 October 2022 – Interpreting figures: NHS Digital; 2022 [Available from: https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/31-october-2022/using-this-publication#top.
- The future of general practice. House of Commons Health and Social Care Committee; 2022-23.
- Clinical academic survey: Medical Schools Council; 2022 [Available from: https://www.medschools.ac.uk/clinical-academic-survey.
- Morgan M, McKevitt C, Hudson M. GPs’ employment of locum doctors and satisfaction with their service. Fam Pract. 2000;17(1):53-5.
Featured image: The future of general practice 2: hidden workers, by Andrew Papanikitas, 2023






Thanks Nada: There are lots if shelves of GPs : academic , executive, managerial , locum, semi-retired, non – patient facing partners. etc etc. What we need it a system that encourages them back into the consulting room without getting burnout !
David Mummery is a GP in West London and a research fellow at the Department of Primary Care and Public Health, Imperial College London
Everything counts , in large amounts: so said the 1983 single by Depeche Mode.2 The same could be said about the next review of the GP contract due in 2024 : for the profession of General Practice, everything counts on this contract, and how it is devised, formulated and implemented.
We have had the chaos recently of the contract imposition; we have had constant discussion and debate about workforce , workload and the possibility of industrial action; we have had GPs leaving and retiring earl , with the ever present reality of burnout for most GPs; we are repeatedly told General Practice is on its knees , and many GPs feel that on a daily basis; we have had numerous articles , workshops, mainstream media debate and other discussion about ‘ the future of General Practice’; we have a disintegrating Conservative Government and a newly re-energised Labour Party waiting in the wings to take over the reigns of Government; we have had the comedian Chris Morris , at the LMC conference giving the single best and funniest talk about General Practice in the history of the profession.3
We GPs should be listening to the Labour Party as they are the ones that are soon going to be in power. We may not agree with Keir Starmer, and Wes Streeting , and what they have recently been saying about General Practice, but we should be listening to them. Keir Starmer’s middle name by the way is Rodney; just a random factoid to try and keep you interested.
Labour is right that the GP partnership model is declining – not in all areas, but certainly in many areas of the country : in some places such as some of the coastal towns of the U.K., many practices rely almost completely on locums. An alternative ‘plan B’ has to be formulated by the BMA and profession as a whole , if the decline of the partnership model proves to be inexorable. It is irresponsible not to plan an alternative path for GPs and general practice.
What might this plan B entail?
There has been talk about GPs being employed by hospitals. This, in my opinion, is a very bad idea and will only formalise the hierarchically inferior, ‘community house officer’ role that many hospital specialists think general practice has become; general practice would lose its independence as a great medical , independent profession. So, no. No mass GP employment by hospitals. Also, secondary care, on the whole does not seem to understand general practice.
Others have talked about going the way of dentistry and essentially leaving the NHS to go private. Seriously? The most vulnerable in our population are pulling their own teeth out with pieces of string because they can’t afford to see a dentist; and free NHS dentistry seems to be unavailable in many areas. Do GPs really want such a system, where only those that have money and can afford it can access care? Is this why we became GPs? So, no. No private large scale model: if individual GPs want to do this, go and work for BUPA or HCA , but don’t impose it on the rest of us, or more importantly the most vulnerable members of the population.
Ok, so that’s no to hospital takeover and no to mass move to private General Practice. So what other models for ‘plan B’ could there be?
Assuming the partnership model is doomed ( which due to unlimited joint and several liabilities in an ever dwindling number of GP partners it is very likely to be: liabilities especially relating to estates will become an increasing problem), what is the best ( or least worst) option for this ‘plan B’ as we go forward: we have already discounted two options .
A third ‘plan B’ option is the rise of the GP super-practices : a corporate model with layers of GP executives and directors and managers etc, performing large scale industrial general practice and ‘patient farming’ of many tens and hundreds of thousands of patients. It is a corporate, capitalist system, aiming for profit for the companies and partnerships involved and likely to want to run the organisation on the cheapest staff possible to maintain and boost profits. We have seen this model spring up across the U.K. in various places, and in some cases the owners are now US health companies. Continuity of care is poor , as generally are patient ratings and feedback and If shareholder owned, then they are beholden to their shareholders. These organisations are generally more keen to employ cheaper staff such as ANPs and physician associates, rather than the more highly-trained GPs who have a much wider and greater clinical experience. This model is not good for GPs or the profession of General Practice or patients: poor ratings, poor continuity of care, exploitation of employees, lack of support for GPs and aiming for profits at all costs could be the norm. No thanks. So that’s another no.
Ok! Plan B mark four – let’s think about this. We need to re-vitalise and re-invigorate General Practice; clinical work must be core and the high risk personally to GPs of doing clinical, patient- facing must be recognised and acknowledged. Payment for GPs has to in some way be linked to clinical work done and thereby clinical risk exposure for all GPs – it isn’t currently in the partnership system. Toxic hierarchies that can exist, have to be abolished in Primary care and flat hierarchies encouraged; one group of GPs should not be the bosses and paymasters to another group and profession should stop being fragmented and divided into : partner, salaried, locum , sessional, portfolio etc. GPs need to be drawn back in from the large locum pool and encouraged to work in teams and groups. Other work such as CPD, teaching , research etc needs to be a visible (and therefore paid) part of a GPs job-plan as it is for a consultant; working 5 or 6 clinical sessions a week should be classed as ‘full time’ and not ‘part time’ as it is by the mainstream media.
So what we need is the invention of a ‘new category’ of General Practitioner. Let’s be old fashioned and just call this new category a ‘GP’ but with no other qualifying features. This new GP will be employed by local authorities or possibly the ICS. This new GP will still be ‘ independent’: the independence of General Practice is not logically linked with the partnership model: in any new system the BMA and LMC must remain as representative and negotiating bodies and funding and form of this must be included in any hard negotiated deal. A good salary must be negotiated; there must be safe workload caps and alert systems ; there must be consultant like job contracts with a PA and SPA type system for job planning, and the SPA time for the CPD, research , teaching , management , special interests etc must be ‘ built’ into the model with for instance 2 SPAs if 5 or more clinical PAs are worked and 1 SPA if less than 5; there must be occupational health for all GPs; the unlimited joint and several liabilities of the partnership model must go. Toxic hierarchies must also go and healthy flat hierarchies of working must be encouraged. Care for patients must remain free at the point of access. This model may be highly appealing to the large number of GPs in the locum pool;4 it may be appealing to some partners and many existing salaried GPs; it will increase the number of ‘patient- facing’ GPs ; it will restore the sense of vocation of General Practice and help it remain the greatest medical profession of all.
As in Charles Lamb’s quote , let us remain a profession who metaphorically ‘lends’ rather than ‘borrows’ like the corporate vultures do: let’s steer well clear if that dangerous road. We and our families are all patients: we need to devise a model that we can proudly say to them we work in, with the best interests of our patients at heart. It should be fun and fulfilling and exciting, patient- facing and sometimes dangerous; not the will-sapping digital dullness that we seem to be living though now.
We can do this. Let’s be proud to call ourselves just general practitioners and make a new system together that will make us, our families, our patients and future generations proud: also, let us once again say with pride, ‘I am a GP’.
References
‘Everything Counts’ song and video, by Depeche Mode, 1983,
[accessed 6/6/23]
Chris Morris, 2023 BMA LMC Conference Speech,
[accessed 6/6/23]
Khan N, https://bjgplife.com/hidden-no-more-the-real-work-of-the-part-time-gps-working-full-time-hours/ [accessed 6/6/23]
Khan N, https://bjgplife.com/the-hidden-shelves-locum-and-academic-gps/ [accessed 6/6/23]
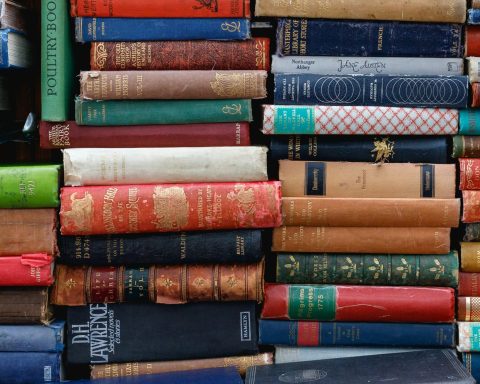
Featured image: Giant Jenga: a metaphor for primary care funding, by Andrew Papanikitas, 2023