The appointment of a practitioner of complementary therapy and healing to the role of medical head of the royal household of the King of England has brought healing into spotlight. Healing, the body’s intrinsic ability to restore optimum functioning, is a dominant theme across complementary and alternative medicine (CAM). Although popular amongst the population1 and becoming more integrated into clinical guidelines,2 CAM has little grounding in dominant science frameworks and is invariably dismissed as a placebo effect. Suggested mechanisms include expectation and reward, conditioning, cognitive and social learning.3 Within the context of clinical trials placebo effects are viewed as a necessary inconvenience which can then be ignored rather than asking: what is going on here and how can we use it to benefit the problem?
In its critique of CAM, medicine may have fallen into the trap of modern physics – a confident assumption that there is one overarching model of reality. In a recent BJGP essay, Misselbrook asks “What has postmodernism ever done for us”?4 We may overlook it at our peril.
A postmodern perspective suggests that any system may have many explanatory models, that they are only ever approximations of reality, and that power and vested interests are never far behind the dominant model. It does not imply that “anything goes,” but is typified by a looser and more abstract conceptual analysis. Explanatory models are viewed as discourses within which individual observations are understood – there is no “grand narrative.” The starting point for healing is: what works for the individual; is there an explanatory story that makes sense; is there potential for harm including failure to explore more effective interventions? A pragmatic approach asks which model seems most appropriate for the context of the task in hand?
A postmodern perspective suggests that any system may have many explanatory models, that they are only ever approximations of reality, and that power and vested interests are never far behind the dominant model. It does not imply that “anything goes…
Healing models
i). The predictive brain and allostatic control.
Whereas homeostatic control seeks to maintain a desired output by negative feed-back, allostatic control seeks to maintain a desired output by predicting what needs to happen to attain it, a feed-forward approach. The accuracy of the predictive model must be continually monitored and predictive error minimised. From a theoretical perspective, this is interpreted as the need to minimise surprise or information entropy, thus resisting a natural tendency to disorder.5
If there is a predictive error, the predictive model of the world is updated. If this is not possible, predictive error can be minimised by modulating ascending sensory inputs .This process takes place in a hierarchical manner with lower levels of the brain dealing with larger predictive errors which if not resolved, are transmitted to higher levels. If the predictive model cannot be updated appropriately, then dysfunctional consequences can result. For example, it has been suggested that stress response to physical or psychological events activate inflammatory mediators which can impact upon the predictive ability of this allostatic mechanism.6 In these circumstances, predictive error is minimised by up-regulating interoceptive signals which can cause distress.
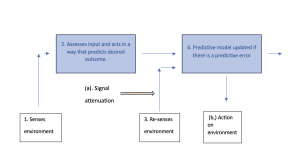
This model also offers an interpretation of some placebo effects – a predictive model re-configuration, resulting in down regulation of interoceptive signals to minimise predictive error with a consequent beneficial effect on sensory input. Specific healing approaches such as hypnosis, visualisation and auto-suggestion may change our predictive models to a more appropriate configuration, allowing minimisation of prediction error without dysfunctional sensory input modulation. Meditative states such as non-sleep deep rest and mindfulness may reduce our dependency on predictive modelling or reduce predictive sampling rate. Alternatively, if greater conscious perception of bodily states can be encouraged using somatic body awareness techniques, interoceptive predictive accuracy may be addressed at an earlier stage at lower hierarchical levels. Figure 1 outlines the principles of allostatic control.
Figure 1. Diagram illustrating allostatic control based on a predictive brain model.
- The brain senses the environment exteroception/interoception.
- Based on experience, the brain predicts the desired action needed to attain a desired outcome.
- The environment is re-sampled, and a predictive error is detected if the desired outcome has not been achieved.
- The predictive model is updated accordingly, and the process is repeated. This occurs in a hierarchy with predictive errors progressively fed to higher levels of the brain.
- If the predictive capacity of the brain is compromised, then predictive error is minimised either by signal attenuation (a) or in extreme cases changing the external environment itself (b).
Complex adaptive systems
Healing can be viewed as facilitating a dynamic harmony between interacting complex systems or complexity matching.
The complexity model views systems from cells to social interactions as a complex network of nested hierarchies containing reiterative interactions with positive and negative feedback loops. These features give rise to nonlinearity – there is rarely a simple relationship between cause and effect and systems cannot be understood by a reduction into their parts.7
Complex systems demonstrate the potential for self-organisation and emergent properties. Patterns evolve that could not have been predicted by an analysis of the component parts and are determined by the application of rules or algorithms acting mainly at a local level. The system adapts by changing its local rules rather than by top-down direction. Although unpredictable in detail, the system follows a trajectory that is bounded and known as an attractor. From a postmodern perspective, we can only ever have a “limited gaze” of any complex system due to difficulties in establishing causality and problematic boundary definition.
Healing can be viewed as facilitating a dynamic harmony between interacting complex systems or complexity matching.8,9 An important concept is self-organised criticality, a state where a complex system can configure itself in an optimum format in response to the demands and constraints placed upon it, enabling it to synchronise with other interacting systems. This state has been identified in a wide range of physical and biological systems including brain and social networks10 and enables the efficient exchange of information and energy utilisation. This could facilitate better allostatic prediction of future states, thereby reducing prediction error. Deviations from health are then viewed as sub-optimal matching of interrelated complex systems.11
The health benefits of nature immersion and socialisation may act in this way, facilitating a greater degree of coherence between the individual and environment. There are also insights for the healing effect of the doctor-patient relationship within the context of a therapeutic consultation. For example, interpersonal interaction demonstrates brain to brain coupling and can alleviate pain.12 The experienced practitioner will demonstrate a perceptual capacity, probing and tuning into the system and matching the complexity of practitioner and patient.13 Sensitised to its nonlinear characteristics, a small input at the correct time can have a therapeutic effect on the system trajectory by changing the patient’s predictive model or system attractor.
Conclusion
A postmodern perspective warns of the dominance of single prevailing explanatory model which is inevitably set in part within constructs of power and vested interests. There can be negative consequences as other theoretical frames and therapeutic opportunities can be dismissed without proper consideration. In line with a postmodern approach, the theoretical models described here offer a fragmented perspective but with a degree of overlap. They may be useful approaches to explore healing and signpost possible interventions that can work alongside traditional approaches.
Perhaps useful first steps would be to replace the term “placebo response” by the “healing effect”, a recognition that the body has its own potential to heal itself if given the appropriate context. And once formal medical trials have established evidence of efficacy, trials conducted with medical interventions alongside complimentary approaches compared with medical interventions alone may be appropriate.
References
- Thomas K , Nicholl J and Fall M. “Access to complementary medicine via general practice.” British Journal of General Practice. 2001; 51.462: 25-30.
- Lewith G , Hyland M, and Gray S. “Attitudes to and use of complementary medicine among physicians in the United Kingdom.” Complementary therapies in medicine. 2001; e 9.3: 167-172.
- Meissner K, Bingel U, Colloca L, et al. The placebo effect: advances from different methodological approaches. Journal of Neuroscience. 2011; Nov 9;31(45):16117-24.
- Misselbrook D. What has postmodernism ever done for us? British Journal of General Practice. 2023 Dec 1;73(737):569-71. DOI: https://doi.org/10.3399/bjgp23X735825
- Friston, K. The free-energy principle: a unified brain theory? Nature reviews neuroscience. 2010;11(2):127-138.
- Borsook D. Understanding migraine through the lens of maladaptive stress responses: a model disease of allostatic load. Neuron. 2012; 73.2 : 219-234.
- Siegenfeld A, Bar-Yam Y. An introduction to complex systems science and its applications. Complexity. 2020; 27;2020:1-6.
- Ashby R. An introduction to Cybernetics. Chapman and Hall. London, 1956.
- Mahmoodi K, West B, Grigolini P. 2019. Complexity matching and requisite variety. arXiv:1806.08808
- Tadić B, Melnik R. Self-organised critical dynamics as a key to fundamental features of complexity in physical, biological, and social networks. Dynamics. 2021; 1(2): 181-197.
- Kernick D. Migraine—new perspectives from chaos theory. Cephalalgia. 2005 Aug;25(8):561-6.
- Goldstein P, Weissman-Fogel I, Dumas G, et al. Brain-to-brain coupling during handholding is associated with pain reduction. Proceedings of the national academy of sciences. 2018 Mar 13;115(11):E2528-37.
- Gillies J, Sheehan M. Perceptual capacity and the good GP: invisible yet indispensable for quality of care. British Journal of General Practice. 2005;55(521): 974-977.
Featured Photo by Kenny Eliason on Unsplash