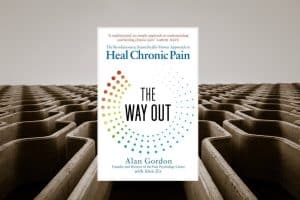
O'Sullivan and others fail to recognise the likelihood that most Long Covid patients will have already tried psychological and behavioural approaches ... the idea that there might be issues that, if addressed, could cure you, is the only thing we have left.
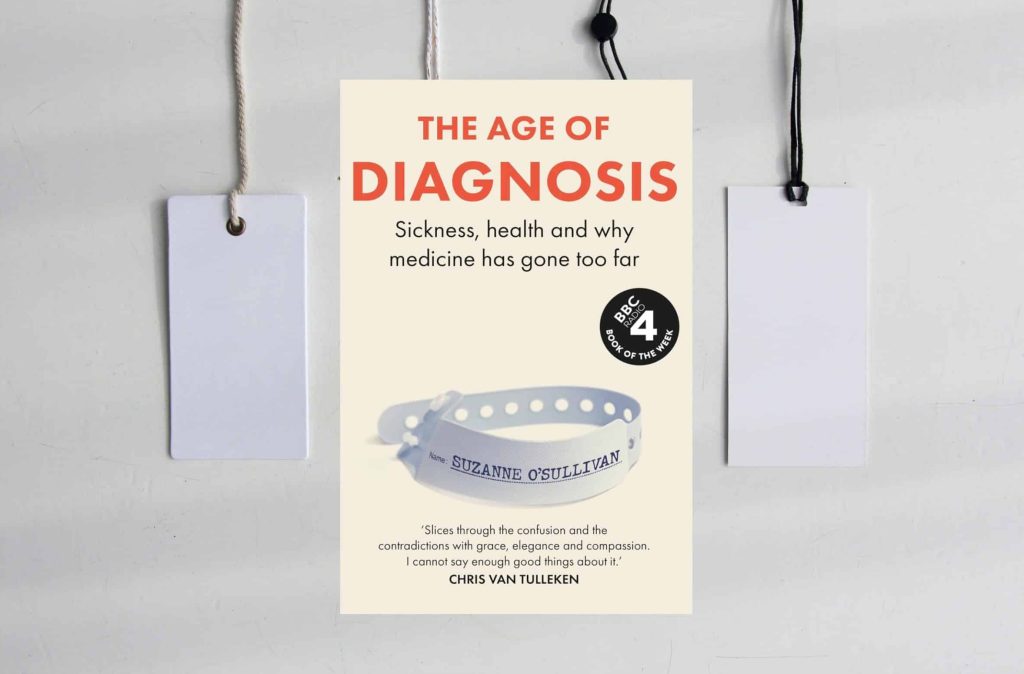
There is much debate in media about whether specific conditions are illnesses, and whether or how they should be treated. Peter Toon considers how these debates inform why we define a condition as illness rather than another type of problem, and the
Taking a look at her consultation model feels like the least painful of her goals to try and get done, and so she takes hold of the flaking metal handrail, slowly breathes in and out to centre herself, and walks down the
Obesity and maintaining a healthy weight are more complicated than excess calories and a lack of exercise. Too often, we are at the mercy of a complex interplay between our genes, personal health matters, the food we eat, the behaviour of those
"Many general practitioners consider spirituality to be relevant to their patients’ health and important to primary care. However, our research showed that a number of GPs worry that addressing this issue is unscientific." Alistair Appleby offers 4 approaches.
With high infection rates and the prevalence of numerous demotivating influences on vaccine uptake, a programme which focusses on negating the controllable barrier of inaccessibility is essential, argue Paul McNamara and Scott Wylie.
"As a GP, I had many patients who told me how lucky they were to be so well in old age. My response was always the same — that they were not lucky but had looked after themselves, mainly by keeping very
"I am struck by how Eder pursued three passions – socialism, Zionism and psychoanalysis – that were all cutting edge causes for most progressive people in his time but have largely diverged from each other since then and become contested or marginalised."
"The Music and Mental Health Project [aims] to sensitise family physicians, other health professionals and managers, as well as patients and their families, to the transformative power of music as a tool for care in psychosocial suffering."
Ponder this: The causal link between our actions and any outcome may be dubious, but the relief we feel at having done something, especially when there is an improvement of some kind, is so strongly reinforcing that we tend to ignore this.
Compassionate care helps us stay connected through our feelings and actions to the human aspect of medicine. And when that feeling is lost, it degrades our sense of who we are as clinicians. Nada Khan considers diagnoses and treatments for compassion fatigue.
Paul McNamara and Khalid Abdalla reflect on sauna therapy for the treatment of chronic disease.
Martyn Hewett and Paquita De Zulueta consider some of the changes that would need to be introduced to safeguard against the most prominent ethical difficulties arising from a change in the law on physician assisted dying.
This challenges the notion that clinical interactions should be structured according to a strict division between diagnosing disease and understanding the patient’s broader illness experience.
In the same way there is an unsettling parallel in the rise of obesity and ultra-processed food from the 1970’s onwards, the rise of faster and more invasive digital technology seems to link with a decline in mental health. Giles Dawnay discusses
What exactly is this smell of poverty? It is so pervasive. I recognise it in an instance. This perfume should be called “Deep End”, and it gives every encounter with poverty a visceral olfactory dimension. Jen Foell reflects.
If it is difficult to agree what exactly we mean by health, it is perhaps unsurprising that we also approach unhealth in a number of different ways. Ben Hoban reflects on the meanings of 'unhealth.'
A recent House of Lords report puts the blame for rising obesity squarely at the feet of the food industry, stating that marketing of unhealthy food products has created an ‘obesogenic’ food environment. Nada Khan investigates the broken food system.
Despite the legal and professional requirements to treat individuals with SpLDs without disadvantage, alongside evidence supporting earlier diagnosis & supportive strategies, the Committee of General Practice Education Directors (COGPED) still do not recommend screening of GP Registrars (GPRs) at the commencement of
"I have often relied on John Driscroll’s three ‘Whats’ when giving feedback on BJGP Life submissions and undergraduate coursework: What happened? So what? What now? I invite you to keep these questions in your head as you survey our articles. How will
Perhaps we can characterise these two kinds of practice as representing either efficiency in providing a high volume of appointments or effectiveness in making each appointment count for more... Ben Hoban reflects.
Primary care has been identified as the stage in the skin cancer pathway with the greatest potential for the use of AI to increase early detection. Richard Armitage raises some issues.
How far have family doctor organisations around the world progressed in protecting planetary health?
The theme for World Family Doctor Day on May 19, 2024, was “Healthy Planet, Healthy People”. To mark this, the World Organisation of Family Doctors’ (WONCA) Working Party on Planetary Health surveyed its 133 member organizations (MOs) across 111 countries. Terry Temple and colleagues
The thread that runs through the debate, however, seems to be a genuine desire on both sides to help people who are suffering, and the conflict between opposing views reflects not a greater or lesser degree of care, but rather the familiar
Doctors are repeatedly referred to in the proposed legislation, and they are clearly essential in delivering the assisted dying process, but has anyone really considered the impact on those doctors? GPs are arguably the most likely profession to provide assisted dying services,
By recognizing the fundamental similarities in our approaches, we can move beyond semantic battles and focus on what truly matters: genuine connection, active listening, and meaningful support for patients.
"In this article, we explore what happens when our automatic ways of being in relationships are no longer serving us well. Moreover, if we can observe what we are doing, is this enough to change things?"
"I couldn’t understand, however, no matter how much I trained, how much I addressed my diet (within the realms of my understanding at the time), and how much I addressed other lifestyle factors such as sleep, why I was the heaviest I
How we understand our story makes a difference to how we go about the job, how effectively we do it, and how it leaves us feeling when we go home... One of these proto-narratives is especially relevant to us as doctors: Overcoming
Aldabra Stifiuc-Andronic and colleagues reflect on the health implications of the cosmetics industry and public awareness of cosmetic ingredients.
"Reducing the carbon footprint of primary care has the potential to improve the health of our patients and communities, while decreasing workload and saving resources ..." – Michael Naughton and colleagues outline what GPs, partners, and local primary care leaders can do to
There is of course no nationwide prostate cancer screening programme for asymptomatic men at present; rather, men over the age of 50 are advised that they can request a prostate-specific antigen (PSA) test from their GP at any time. Paul McNamara and
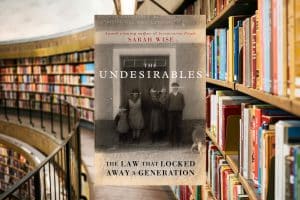
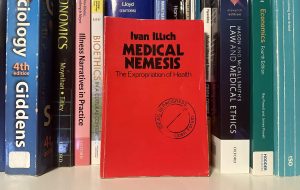
"This book is terrifying, informative, stimulating, and educating to every member of the medical and nursing profession. It is extensively researched, has a massive bibliography, and, most importantly, it is well written and well worth reading — in spite of some truly
Re-reading my review, I can tell that I was very careful even then not to present this approach as a 'cure' for Long Covid, but as a promising approach to manage symptoms better while waiting for a cure ... However, I have
For years, the UK has inaccurately perpetuated the notion that British farming is among the most sustainable globally. Shireen Kassam, Christelle Blunden and Matthew Lee argue why this is not so, and the impact this may have on public and planetary health.
"The body does not generate the mind but is a process of self-localisation of the mind itself ..." – Armando Henrique Norman explores the usefulness of idealism as a valid philosophical principle to guide family physicians in their daily practice.
a book which has had the same impact on the language of healthcare as George Orwell’s 1984 has had on the language of politics. Illich did not invent terms such as iatrogenesis and medicalisation, but he was the first to synthesize them
Identifying the mind as a source of the body's pain can help a patient make great strides towards taking control of their health and reducing the impact chronic illness has on their day to day lives. Paul McNamara and Ella Butterworth explore
Clearly in some GP Practices no robust thought has been given to having a Mental Health Practitioner (MHP), or their role and scope of practice. Those GPs who have requested and take 'ownership' of the MHP, are best placed to integrate them
Despite regular reports about ‘improving the diet of the population’, little has changed. Eight years ago less than a third of people ate five portions of fruit and vegetables per day, and that figure hasn’t budged since. Chris Newman suggests that GPs