
He is on Twitter: @JamesMaloneLee3
How often do you meet a patient who describes symptoms of urinary tract infection (UTI) but the urinalyses, whether dipsticks or culture, prove negative? Have you noticed the increasing numbers of predominantly women who keep re-presenting with lower urinary tract symptoms (LUTS) that defy the advice of the tests that you use? You are doing right by the guidelines and you have taken note of the contemporary concerns about antimicrobial resistance (AMR). These patients are baffling aren’t they? The specialists write about “painful bladder syndrome” (PBS), renamed “bladder pain syndrome” (BPS) or “interstitial cystitis”. So, the patients are ultrasounded, CT and MRI scanned. They are urodynamicked, cystoscoped, bladder-stretched, urethra-dilated and then instilled with various concoctions, but frustratingly still they return.
This perplexing problem has been my obsession for forty years, and with our happy gang of researchers it would seem that we have come up with some useful answers. Today we have sufficient knowledge for me to write a book about it, “Cystitis Unmasked” (see below), that is pitched at clinicians and informed patients alike. There is quite a story because our science found that the guidelines and urinalyses methods were incorrect. That is a gentle adjective because the truth is that they are calamitously wrong. However, we have learned that reporting such science to power is a tricky business. We have spent a decade deflecting a string of criticisms by the chaps in charge who seemed outraged by the outcomes of our science. Feelings ran so high that we felt obliged to conduct the studies necessary to address every proposition that was floated to explain away what we were trying to report. Thus, we evaluated one “no true Scotsman” argument after another in a dispiriting sequence of negative experiments. However, today I may report that the original findings have weathered a hugely detailed critical scrutiny, so we have some confidence in what we have published.
Our science found that the guidelines and urinalyses methods …. are calamitously wrong.
The normal bladder is not sterile but hosts a complex polymicrobial microbiome of several hundreds of different species, and a 95% overlap with patients who have UTI.5 There is no truth in the claim that the microbe isolated by a midstream urine culture (MSU) is the proven causative organism. The problem of causation is unresolved and applies equally to enhanced cultures and genomic methods. We may isolate microbe(s) but we haven’t a clue whether they are friend or foe. If you treat on the sensitivity data obtained from a culture you are more likely to fan the flames of antimicrobial resistance (AMR) than treat the patient successfully.6,7 Simple, narrow-spectrum, urinary antibiotics in sufficient dose will perform just as well with less AMR. “Mixed growth of doubtful significance” is of considerable significance in reflecting the pathology of UTI.2 The epithelial cells identified in urinalyses are not indicators of contamination but important biological manifestations of active cystitis.8
Simple, narrow-spectrum, urinary antibiotics in sufficient dose will perform just as well.
This is all most worrying. The science has been done carefully and additional work has been achieved to address the common arguments that have been used to claim that none of this could be true. The time has come for those who have the relevant influence to insist that the guidelines and regulations should be re-examined in the light of this new knowledge. It is most unfair on the patients to do otherwise.
To conclude, please consider two images. The first is a confocal micrograph (the picture at the top of this article) achieved by Dr Harry Horsley PhD, a most gifted researcher in our centre. It shows urothelial cells extracted from a urine sample and reveals microbes adherent to the surfaces of these cells, but others parasitising these unfortunate cells in order to set up a chronic infection that will be hard to eradicate. This is the pathology that explains those patients who keep returning to you with recalcitrant symptoms but negative tests.
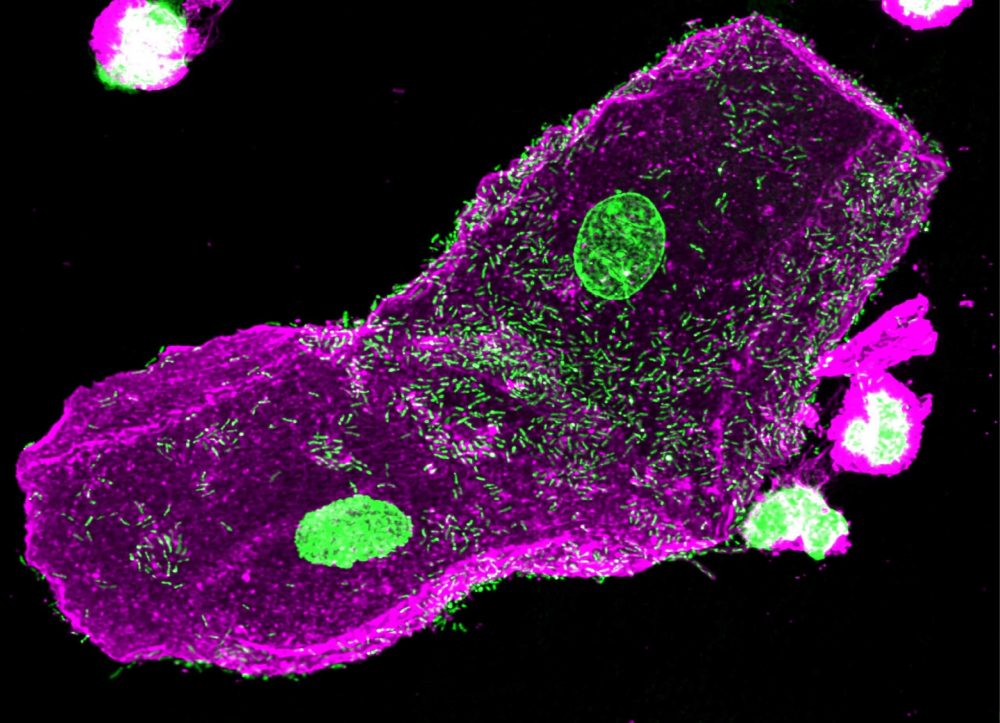
The second is the graph (right) of the NHS returns for admissions for IC/PBS/BPS annually since 1998. 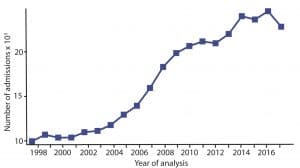
James Malone-Lee’s book is “Cystitis Unmasked”. TFM Publishing Ltd (1 Feb. 2021) ISBN-13 : 978-1910079638 His author royalties will be donated to the current research programme at UCL.
References
- Kupelian AS, Horsley H, Khasriya R, Amussah RT, Badiani R, Courtney AM, et al. Discrediting microscopic pyuria and leucocyte esterase as diagnostic surrogates for infection in patients with lower urinary tract symptoms: results from a clinical and laboratory evaluation. BJU Int 2013; 112(2): 231-8.
- Sathiananthamoorthy S, Malone-Lee J, Gill K, Tymon A, Nguyen TK, Gurung S, et al. Reassessment of routine midstream culture in diagnosis of urinary tract infection. J Clin Microbiol 2019; 57(3): 01452-18.
- Gill K, Kang R, Sathiananthamoorthy S, Khasriya R, Malone-Lee J. A blinded observational cohort study of the microbiological ecology associated with pyuria and overactive bladder symptoms. Int Urogynecol J 2018; 29(10): 1493-500.
- Khasriya R, Barcella W, De Iorio M, Swamy S, Gill K, Kupelian A, et al. Lower urinary tract symptoms that predict microscopic pyuria. Int Urogynecol J 2018; 29(7): 1019-28.
- Hilt EE, McKinley K, Pearce MM, Rosenfeld AB, Zilliox MJ, Mueller ER, et al. Urine is not sterile: use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol 2014; 52(3): 871-6.
- Swamy S, Barcella W, De Iorio M, Gill K, Khasriya R, Kupelian AS, et al. Recalcitrant chronic bladder pain and recurrent cystitis but negative urinalysis: what should we do? Int Urogynecol J 2018; 29(7): 1035-43.
- Swamy S, Kupelian AS, Khasriya R, Dharmasena D, Toteva H, Dehpour T, et al. Cross-over data supporting long-term antibiotic treatment in patients with painful lower urinary tract symptoms, pyuria and negative urinalysis. Int Urogynecol J 2019; 30(3): 409-14.
- Horsley H, Malone-Lee J, Holland D, Tuz M, Hibbert A, Kelsey M, et al. Enterococcus faecalis subverts and invades the host urothelium in patients with chronic urinary tract infection. Plos One 2013; 8(12): e83637.
- Zalmanovici TA, Green H, Paul M, Yaphe J, Leibovici L. Antimicrobial agents for treating uncomplicated urinary tract infection in women. Cochrane Database Syst Rev 2010; (10): CD007182.
- NICE. Urinary tract infection (lower) – women. London: National Institute for Health and Care Excellence, 2014. Available from: http://cks.nice.org.uk/urinary-tract-infection-lower-women#!topicsummary.
Featured photo by Dr Harry Horsley, courtesy of the author.


As a sufferer of UTIs for more than two decades, the situation can seem bleak. To know you have a raging infection and be repeatedly told by GPs, relying on unreliable testing methods and outdated treatment guidelines, that you do not, is both frightening and infuriating. I really hope things change soon.
My daughter has been suffering from this since the age of 12, she’s now 26. She’s had every procedure you mentioned all to no avail. We always thought the infection was like a ghost hiding somewhere just to reappear. 🙏
As a sufferer of 44 years and still counting, I have had most of the above, although never offered CT or MRI scans, I find it so frustrating, only just found out, by myself about embedded uti’s. As I get older, now 62, it is more frightening as I’m still not being believed, after all these years of knowing my body and my symptoms of infection, I did expect things to change over the years but it hasn’t. We do need help.
4 yeras under treatment with urologist has no avail but after knowing the secret behind of chronic uti as Prof. James Malone Lee has mentioned and with that followed his protocol of long term course of antibiotics has saved my life ! Thank you Prof. God bless you
4 decades of recurrent UTI infections, a number of them not showing up on dipstick / path lab tests, leading to disbelief by urologists and Drs, despite my ongoing bladder pain. Repeated short courses of antibiotics; numerous cystoscopies ;bladder stretches; ultrasounds,flow tests and so on. None of the interventions gave me any symptom relief and I was eventually labelled as having Interstitial Cystitis. I I was finally discharged with a letter identifying me as ‘ a complex case’ . I was even advised to consider a referred for TVT surgery as this ‘may help’. Eventually, 4 years ago, I was treated by Professor Malone Lee. The antibiotic treatment regime gave me my life back. This horrendously painful condition is afforded such low priority in the NHS and often dismissed by urologists and GP’s because outdated standardised tests don’t often show an infection. .After decades of continually struggling with bladder infections and being disbelieved when urine tests were negative despite my pain, I’m now 90 % better under Professor Malone Lee’s treatment regime. Antibiotics aren’t ideal long term but it’s all most of us have to keep us from Sepsis, until the government listen and afford more funding and resources to researching this highly under sourced condition.