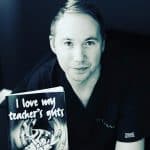
 Paul McNamara is a GP in Glasgow and honorary clinical lecturer at the University of Glasgow. He has an interest in research and medical education. He is the author of three books: ‘I Love My Teacher’s Guts’, ‘Case-based Discussions in Medicine’, and ‘Mastering Medical Exams’.
Paul McNamara is a GP in Glasgow and honorary clinical lecturer at the University of Glasgow. He has an interest in research and medical education. He is the author of three books: ‘I Love My Teacher’s Guts’, ‘Case-based Discussions in Medicine’, and ‘Mastering Medical Exams’.
Sarah Gray is a 4th year medical student at the University of Glasgow. She has a passion for primary care and aspires to be a GP.
The cost-of-living crisis is descending like a dark cloud and its heavy weight is palpable. As a Deep End GP, every day I see the real impact poverty is having on my patients. I’ve been seeing an increasing number of patients present with a deluge of issues such as malnutrition and the negative impact that cold and damp housing is having on physical symptoms and subsequent ill health.
As a practice, we have seen patients preferentially choosing telephone appointments over face-to-face because they can’t afford transport to the surgery, and last week I had to use £40 from our petty cash to pay for a taxi for a patient that I referred to secondary care who had no means of paying themselves, and whom didn’t warrant ambulance transfer. We are also bearing witness to the emerging two-tier service that is evolving with my patients having no hope of ever being able to afford private health care and subsequently suffering due to prolonged secondary care waits.
“… those in the lowest income decile spend 90% of their income on essential spending”
Recently the Bank of England published a report stating that those in the lowest income decile spend 90% of their income on essential spending,1 which includes household maintenance, utility bills, taxes, groceries, transport, and communication. This is twice the proportion that the highest income decile is spending on their essentials.
Having such high expenditures on essential spending leads to individuals in the lowest income decile being unable to place money in savings, meaning they are less able to cope with unexpected costs or sudden rises in bills.1,2 The essential spending does not include costs for other requirements such as prescription charges and clothing, meaning that the financial situation for the most vulnerable may be even worse than these figures suggest.
The impact of the cost-of-living crisis not only affects how much money people have but also negatively impacts their health.3 Health is affected by a complex web of many factors.4 Some are down to an individual’s lifestyle, but many are socioeconomic. Increasing deprivation has been linked to increased levels of chronic disease across Europe,5 with conditions such as cardiovascular disease, type 2 diabetes, and depression all showing increased prevalence in areas of low socioeconomic status.6–9 Almost every day, I see a new diagnosis of type 2 diabetes and I have lost count of the number of low folate bloods I have signed off and treated. But there are real people behind these blood results, and their stories of choosing whether to heat their homes or feed their hungry children are heart-breaking.
As the cost-of-living crisis progresses, how will this impending tsunami of increased demand impact an already stretched and over-burdened primary care service? We asked 185 colleagues in an informal survey via GP social media groups what the cost-of-living crisis meant for primary care.
“… 97% [of survey responders] said they were worried about the financial stability of non-clinical staff in their practice … “
Perhaps unsurprisingly, colleagues reported that the cost-of-living crisis was a significant issue throughout primary care, with 86% of responders seeing an increase in mental health presentations and 66% seeing an increase in physical health presentations related to the crisis. Overall, 82% said their workload had increased due to the cost-of-living crisis, and 78% noted their patients have had to stop activities and hobbies that are beneficial to their health.
It is known that increased workload in primary care leads to a decline in mental health.12,13 Our findings echo this, with 58% saying their mental or physical health has been affected by the cost-of-living crisis. Sadly, 64% of responders reported they were facing personal financial concerns due to the cost-of-living crisis.
The cost-of-living crisis means that fuel and energy costs are increasing,2,17 so practices are becoming more expensive to run and staff require an increase in salary to account for inflation.18 In total, 97% said they were worried about the financial stability of non-clinical staff in their practice, with 72% of GP partners reporting they were making changes to staff wages.
Primary care appears to be struggling and there is genuine concern about how we will manage the increasing demand placed on us by the cost-of-living crisis. We need to advocate, lobby, and collaborate for our most vulnerable patients and together we may yet weather the storm.
References
1. Bank of England. Financial stability report — July 2022. 2022. https://www.bankofengland.co.uk/financial-stability-report/2022/july-2022 (accessed 16 Dec 2022).
2. Office for National Statistics. The rising cost of living and its impact on individuals in Great Britain: November 2021 to March 2022. 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/expenditure/articles/therisingcostoflivinganditsimpactonindividualsingreatbritain/november2021tomarch2022 (accessed 16 Dec 2022).
3. Limb M. Failure to protect cost of living will increase poverty and health inequalities, warn analysts. BMJ 2022; 376: o794.
4. Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health. Background document to WHO — strategy paper for Europe. 2007. https://ideas.repec.org/p/hhs/ifswps/2007_014.html (accessed 16 Dec 2022).
5. Dalstra JAA, Kunst AE, Borrell C, et al. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol 2005; 34(2): 316–326.
6. Jackson CA, Jones NRV, Walker JJ, et al. Area-based socioeconomic status, type 2 diabetes and cardiovascular mortality in Scotland. Diabetologia 2012; 55(11): 2938–2945.
7. Wildman J. Income related inequalities in mental health in Great Britain: analysing the causes of health inequality over time. J Health Econ 2003; 22(2): 295–312.
8. Skapinakis P, Lewis G, Araya R, et al. Mental health inequalities in Wales, UK: multi–level investigation of the effect of area deprivation. Br J Psychiatry 2005; 186(5): 417–422.
9. Ostler K, Thompson C, Kinmonth AL, et al. Influence of socio-economic deprivation on the prevalence and outcome of depression in primary care. Br J Psychiatry 2001; 178(1): 12–17.
10. British Medical Association. Caring for the mental health of the medical workforce. 2019. https://www.bma.org.uk/media/1365/bma-caring-for-the-mental-health-survey-oct-2019.pdf (accessed 16 Dec 2022).
11. Karuna C, Palmer VJ, Scott A, Gunn J. Prevalence of burnout among general practitioners: a systematic review and meta-analysis. Br J Gen Pract 2022; DOI: https://doi.org/10.3399/BJGP.2021.0441.
12. Pettinger T. Causes of the cost of living crisis explained. 2022. https://www.economicshelp.org/blog/170481/economics/causes-of-the-cost-of-living-crisis-explained (accessed 16 Dec 2022).
13. Hourston P. Cost of living crisis. 2022. https://www.instituteforgovernment.org.uk/explainers/cost-living-crisis (accessed 16 Dec 2022).
Featured photo by Siora Photography on Unsplash.






