Rodney Jones is a retired Chartered Management Accountant and a Statistical Advisor providing advice to NHS organisations in forecasting demand and capacity planning. His publications can be accessed at: https://www.mdpi.com/1660-4601/20/24/7171/s1.
All countries have a population-based resource allocation formula that distributes resources and finances to different parts of the country.1 There are probably as many formulae as countries or federal states. This diversity reflects differing opinions regarding ‘need’ and how to model ‘need’. All will claim that their formula is the ‘best’ and ‘fairest’ possible. Financial risk arises from the gap between the real costs and those predicted by the resource allocation formula. The recipient of the formula-based ‘fair’ share is responsible for managing the gap. Since it is far harder to modify emergency admissions, the gap must then be ’managed’ by attempts to triage GP referrals, reduce elective demand, limit drug costs, etc.
I have lost count of the number of resource allocation formulae applied in England, each claiming to surpass those that came before. No one ever mentions that all models can fail because of hidden assumptions. I observe that, in England and elsewhere, the key hidden assumption is that population age is the fundamental determinant of health costs, which is modified by multiple factors to determine local ‘need’.
I have lost count of the number of resource allocation formulae applied in England, each claiming to surpass those that came before. No one ever mentions that all models can fail because of hidden assumptions.
However, for over 40 years economists have known that it is nearness to death (NTD) rather than age per se that drives an individual’s lifetime healthcare costs.2 In NTD, death is the key point of reference, from which costs are determined by counting backward. For example, some 55% of lifetime hospital bed usage occurs in the last year of life 3 Age and morbidity do determine some costs; however, NTD is the primary driver.2 To omit death as a key variable will then cause even the most complex formula to fail. Why has NTD never been incorporated into the English resource allocation formula? If the absolute number of deaths each year is so important, how may this affect the unexpected changes in year-to-year costs experienced by English Integrated Care Boards (ICBs)?
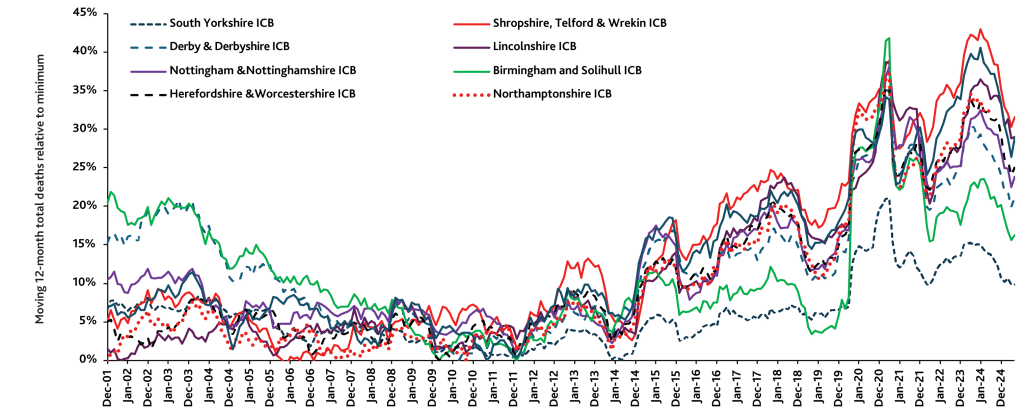
Figure 1 presents a fascinating insight, where the number of monthly deaths in each ICB since 2001 was estimated based on the constituent local authorities.4 ICB deaths are available from 2024,4 and these estimates were normalised to the actual deaths in the first 3 months of 2024. The estimates are usually close to the actual ICB deaths. Small differences are due to ICB populations based on patients registered with a GP practice rather than residents in a local authority. The monthly deaths were summed into a moving 12-month total and presented relative to the minimum 12-month total since 2001. Eight ICBs were chosen to illustrate the complexity of the trends using deaths as a retrospective measure of NTD costs occurring in the last year of life for each ICB.
The trends are very complex, involve periods of unexplained high or low deaths, and are likely to be influenced by infectious outbreaks. On this occasion, the Birmingham and Solihull ICB was most affected by COVID-19 while South Yorkshire ICB was far less so. With 3000 known species of human pathogens,5 such complex trends are to be expected. All human pathogens inadvertently modify the profile of noncoding RNAs (ncRNAs) as part of the process of pathogen interference,5 which modifies both immune and other gene expressions in complex and unpredictable ways.6
… for over 40 years economists have known that it is nearness to death (NTD) rather than age per se that drives an individual’s lifetime healthcare costs.
The key point is that, while projected costs based on population age profiles follow smooth trajectories, those for deaths, and so costs, do not. Each ICB has a unique time profile that is only vaguely estimated from actuarial methods — which also have yet more hidden assumptions.
Further to the issue of hidden assumptions in wider resource allocation, the number of deaths is also vital to understanding the demand for hospital beds — possibly because infections per se, including those of an apparent asymptomatic or sub-acute nature, may give the nudge that precipitates an acute admission for seemingly unrelated diagnoses.7
It has been proposed that the actual number of deaths, adjusted for the cause of death, must be used as a retrospective adjustment to ensure that all ICBs receive a genuine fair share of available funds.8 Failure to do so will lead to unforeseen and unpredictable financial pressures for which ICBs will be unjustly held accountable. Patients and their GPs will then suffer from the resulting (futile) attempts to balance the budget.
References
1. Johnston BM, Burke S, Kavanagh PM, et al. Moving beyond formulae: a review of international population-based resource allocation policy and implications for Ireland in an era of healthcare reform (version 1; peer review: 1 approved, 1 approved with reservations). HRB Open Res 2021; 4: 121. https://doi.org/10.12688/hrbopenres.13453.1 (accessed 26 Jul 2024).
2. Moore PV, Bennett K, Normand C. Counting the time lived, the time left or illness? Age, proximity to death, morbidity and prescribing expenditures. Soc Sci Med 2017; 184: 1–14. https://doi.org/10.1016/j.socscimed.2017.04.038 (accessed 26 Jul 2024).
3. Hanlon P, Walsh D, Whyte BM, et al. Hospital use by an ageing cohort: an investigation into the association between biological, behavioural and social risk markers and subsequent hospital utilization. J Public Health Med 1998; 20(4): 467–476.
4. Office for National Statistics. Deaths registered monthly in England and Wales. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/monthlyfiguresondeathsregisteredbyareaofusualresidence (accessed 26 Jul 2024).
5. Jones RP, Ponomarenko A. Roles for pathogen interference in influenza vaccination, with implications to vaccine effectiveness (VE) and attribution of influenza deaths. Infect Dis Rep 2022; 14(5): 710–758. https://doi.org/10.3390/idr14050076 (accessed 26 Jul 2024).
6. Acuña SM, Floeter-Winter LM, Muxel SM. MicroRNAs: biological regulators in pathogen–host interactions. Cells 2020; 9(1): 113. DOI: 10.3390/cells9010113.
7. Jones RP. Addressing the knowledge deficit in hospital bed planning and defining an optimum region for the number of different types of hospital beds in an effective health care system. Int J Environ Res Public Health 2023; 20(24): 7171. https://doi.org/10.3390/ijerph20247171 (accessed 26 Jul 2024).
8. Jones R. Multidisciplinary insights into health care financial risk and hospital surge capacity, Part 4: What size does a health insurer or health authority need to be to minimise risk? J Health Care Finance 2021; 47(3): 1–23.
Featured Photo by Sarah Agnew on Unsplash







One of the most insightful and relevant articles I have read in years
Thank you for your kind words. I have spent 30 years researching the issue of both financial and capacity risk in healthcare. The simple conclusion is that demand jumps around so much that reality is incompatible with the simplistic ‘average’ or ‘steady state’ assumptions that the politicians and their proxies assume ‘must’ or ‘ought’ to apply to the NHS. The NHS then gets cruelly blamed for their ‘inability’ to manage demand. As they say, a picture is more eloquent than a thousand words. There is a follow-on piece about how to correctly fund the NHS coming out in a couple of weeks.