The June 2023 issue of BJGP focuses on primary care systems, and the selection of articles in Life and Times celebrates the often–overlooked details of what happens within them, what influences them and what wider influence they might have. Primary care systems can clearly be described as networks of people and things, ideas, processes, relationships and technologies. Where do we start? Social scientists often use a social theory as a lens or filter for seeing through the chaotic fog of everything happening at once. Actor Network Theory (ANT), for example, has been handily summarised by Greenhalgh and Stones (2010), in their discussions of big information technology programmes in healthcare.1 ANT considers networks made up of both people and technologies.2,3 ANT focusses on what people and things become as a result of their position in a network and the dynamic configurations of human and non-human actors. Actor-networks are often highly dynamic and inherently unstable. They can stabilise to some extent when people, technologies, roles, routines, training, incentives, and so on are aligned. This alignment is attempted in four stages: problematisation (defining a problem for which a particular technology is a solution), interessement (getting others to accept this problem-solution), enrolment (defining the key roles and practices in the network), and mobilisation (engaging others in fulfilling the roles, undertaking the practices and linking with others in the network).2 The tricky question here is whether we consider primary care systems to be networks or the solution to a problem within a network.
The ghosts in the machine
Our book reviews in June 2023 reflect the the relevance of seeing and understanding the ecosystem we inhabit and its constituent elements, including us! I review a beginners’ guide to economics and find that many of the ideas describe the trials and tribulations of practitioners and patients.4 Trisha Greenhalgh reflects on an edited collection that showcases application of ‘mindlines’ in medical practice.5 These are the strains, interests, concerns and relationships that are the stuff of interssement and mobilisation. Ben Hoban reviews the work Dilys Daws and learns how to be quietly disruptive: this can mean resisting the pressure to ‘do’, and listen instead.6 David Misselbrook finds that new paediatric text is a source for shared understanding between generalists and specialists – surely a recipe for a healthy primary and secondary care interface.7
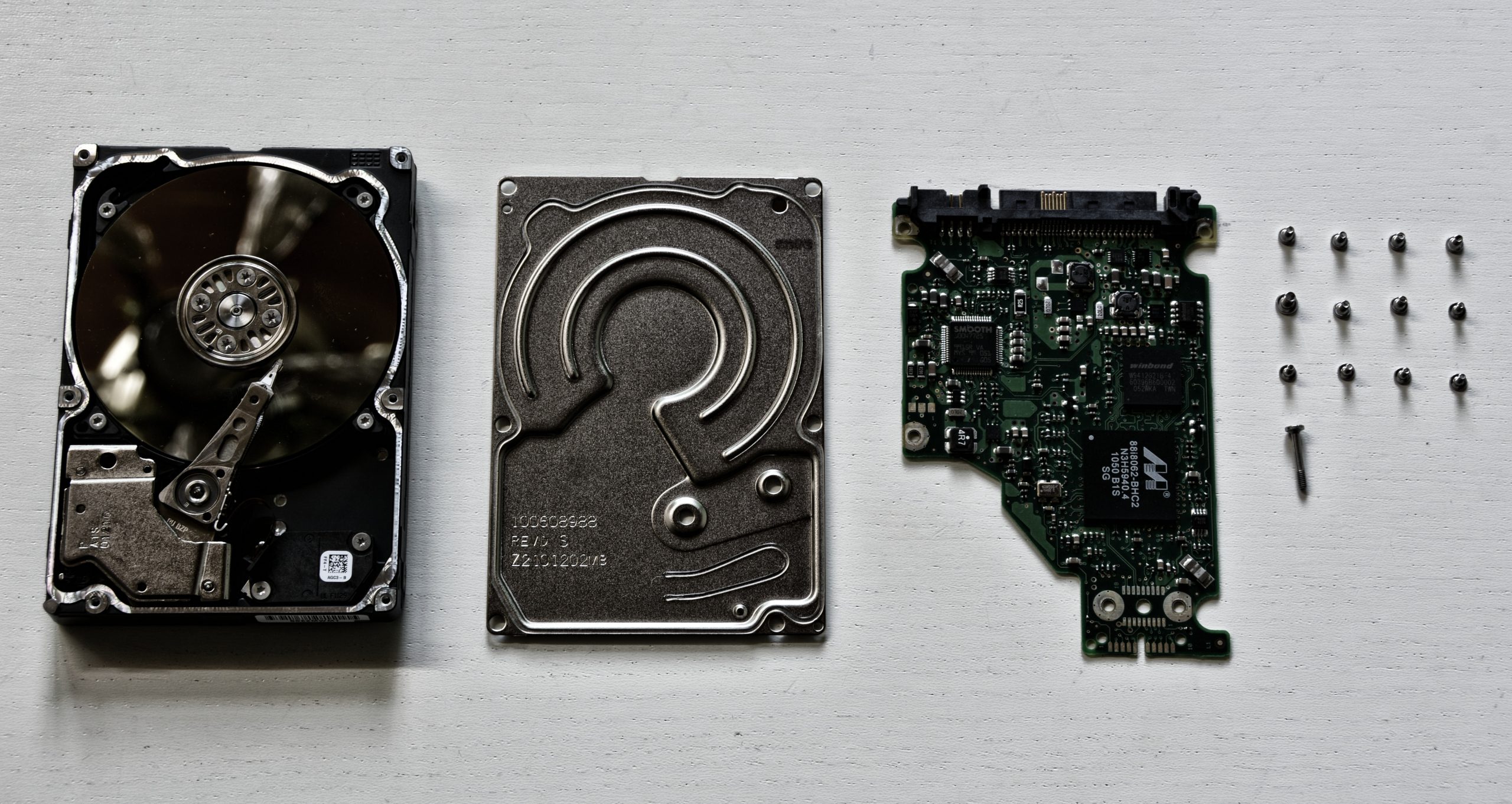
The devil in the details
It is patently clear that we have a duty open the black boxes of our primary care systems…
Value for money to the person (or institution) that pays remains a powerful motivator in these times. Nada Khan asks the question of how much of todays money a GP costs to make? How much of that cost is born by the state and how much is born by the GP themselves?8 The problem with this lies not only in capturing the truest financial costs incurred, and benefits recouped in creating a GP, but also in identifying the moral and political value of this investment. Richard Armitage raises what should be a ‘straw man’ (an argument that is easy to knock down)of informed consent as an exercise in form–signing rather than exploration of agreement to the nature and purpose of a medical treatment.9 The worry is that in these pressured, automated times, systems may abhor poor consent, but they do not value the understanding that leads to good consent. The passive verb, ‘consenting,’ serves as an ethical oxymoron, it is something done to rather than with the patient. Ahmed Rashid regales us with more diverse wisdom from the field: female genital mutilation, hand hygiene, monitoring supervised consumption services, and caring masculinites are this month’s selection.10
Notes from a profession in a misaligned system
Has British general practice always been in crisis? Emilie Couchman reflects on the 1950 Collings report in the lancet. His damning report galvanised British general practice.11 However, one must only catch a glimpse of the news to realise that GPs are clearly still working within a system that is misaligned both for its workers and its end users. To this end, Lara Shemtob and her fellow academic clinical fellows set out a manifesto for for a sustainable workforce. The people factors are the strongly positive aspects of the job. But the logistical working conditions must improve for the future of the specialty to be sustainable.12 General practice exists ‘as’ and ‘in’ a network with dynamic relationships between human and non human actors. Rebecca Quinn express the misalignments of primary care more lyrically as a poem, ‘My heart goes out to all of us, who have been ‘set up to fail’. Take heart and glove up – the work must go on…’13
It is patently clear that we have a duty open the black boxes of our primary care systems, lest ignorance of how they work (and how they can work) destroys them and the good that they do. Nye Bevan is widely quoted as saying ‘The NHS will last as long as there’s folk with faith left to fight for it.’14 Faith helps, but it may not be enough.
References