Richard Armitage is a GP and Clinical Lead affiliated with the Division of Epidemiology & Public Health at the University of Nottingham. He is on Twitter: @drricharmitage
Richard Armitage is a GP and Clinical Lead affiliated with the Division of Epidemiology & Public Health at the University of Nottingham. He is on Twitter: @drricharmitage
One notable impact of the COVID-19 pandemic in the UK was a dramatic reduction in both the number of Two Week Wait (2WW) referrals being made by general practitioners, and the number of patients being diagnosed with and treated for cancer. This combination reflects an outstanding burden of undiagnosed malignant disease which, according to trends in NHS data, now seems poised to imminently present to the health service.
….a dramatic reduction in both the number of Two Week Wait referrals ….and the number of patients being diagnosed with and treated for cancer.
NHS England publishes monthly data on the waiting times of people referred from primary care with suspected cancer and those subsequently beginning treatment.1 The monthly number of 2WW referrals made during the first COVID-19 lockdown was up to 59.1% lower than the preceding seven-month average (reflecting all available data), before returning to its pre-lockdown level in July 2020, and remaining stable since. The monthly number of patients receiving first treatment for a new cancer diagnosis was up to 36.2% lower than the preceding seven-month average, before returning to its pre-lockdown level in September 2020, and remaining stable since. Crucially, despite both returning to baseline, neither rate has risen above its respective pre-pandemic level.
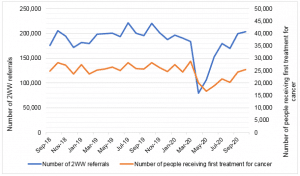
The simultaneous reduction in both 2WW referrals and new cancer diagnoses implies that a proportion of the ‘missed’ referrals included patients with undiagnosed cancer. Without intervention, these tumours would progress until the associated symptoms become severe enough to trigger medical help-seeking, ultimately leading to a delayed diagnosis and initiation of treatment. This would be reflected in the rates of 2WW referrals and new cancer diagnoses rising above their respective baselines, as these missed tumours are managed in the health service alongside the on-going monthly burden of suspected and newly diagnosed cancer (which would not change). However, while the rates of 2WW referrals and new cancer diagnoses have returned to baseline, neither have risen above their pre-pandemic levels. This suggests an outstanding burden of thousands of undiagnosed cancers continues to exist.
An alternative explanation is that the delay in new cancer diagnoses caused patient death or rendered these tumours untreatable, meaning they do not appear in the first treatment statistics, although this is unlikely to explain the entirety of the outstanding disease burden generated within this period of time.2 It is more likely that the low rate of new cancer diagnoses results from the low rate of 2WW referrals due to patients with signs of cancer not consulting with primary care during the COVID-19 lockdown.
….new cancer diagnosis rates suggest the imminent arrival of an influx of undiagnosed cancer into the health service.
The return to baseline of the 2WW referral and new cancer diagnosis rates suggests the imminent arrival of an influx of undiagnosed cancer into the health service. Accordingly, primary care practitioners should prepare to send above-average numbers of 2WW referrals, and not be deterred from doing so by the impact of COVID-19 on a health service entering the winter season. Concurrently, NHS cancer services should prepare to receive an above-average caseload consisting of disproportionate levels of advanced disease, while public health practitioners should strengthen cancer awareness campaigns to educate patients in the recognition of concerning symptoms and timely medical help-seeking.
References
- NHS England. Cancer Waiting Times. https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/ [accessed 03 January 2021]
- C Maringe, J Spicer, M Morris, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. The Lancet Oncology 01 August 2020; 21(8): 1023-1034. DOI: 10.1016/S1470-2045(20)30388-0
Featured photo by National Cancer Institute on Unsplash