‘Some experts’, the BBC news story reads, ‘are asking for do not resuscitate orders to be scrapped’ as they are being misused and putting people’s lives at risk. This is, understandably, a highly emotive topic for patients, their families, and for health care professionals. Do not attempt cardiopulmonary resuscitation (DNACPR) orders guide others not to attempt CPR when patients don’t want it, or when it’s unlikely to be successful. Many secondary care trusts have moved away from stand-alone DNACPR forms towards a more holistic approach to patient preferences and care planning. What is happening in general practice to ensure DNACPR and treatment escalation plans are taking into account patient, carer, and clinicians voices?
What is happening in general practice to ensure DNACPR and treatment escalation plans are taking into account patient, carer, and clinicians voices?
The Tracey vs. Cambridge University Hospitals NHS Foundation Court of Appeal decision in 2014 changed the recommendations around how and when DNACPR orders need to be discussed with patients. The final judgement in the case means that clinicians need to discuss DNACPR decision making with patients, or if they do not have capacity to be involved with the decision making process, with a legal proxy or the patient’s family or friends. Following these discussions, the decision to issue a DNACPR order lies with the treating clinician, but if the patient or family disagree with this decision, a second opinion should be sought, but this is not a legal obligation.1 But the essence of this case, and the Carl Winspear case in 2015, was that patients with capacity to be involved in DNACPR consultations need to be involved before decisions about resuscitation are put in place. Despite this guidance, it’s not clear if this is happening in practice across all settings. The BBC news story reported on a study conducted in care homes during the Covid pandemic to look at implementation of DNACPR recommendations and their use in that setting.2 Concerningly, in this study, 56% of health care professionals in care homes had witnessed DNACPR forms put in place without consultation with the resident or their family, going directly against the recommendations from the Tracey judgement.
A move towards ReSPECT forms
At least in the UK, most hospital trusts have been moving away from the old ‘red form’ DNACPRs and instead taking on more detailed treatment escalation planning through the Recommended Summary Plan for Emergency Care and Treatment, or ReSPECT form. The ReSPECT process was developed in part as a response to variation and sub-optimal practice in DNACPR discussions, decisions, and interpretation, and as a way to better record patient preferences for broader emergency care and treatment.3 This is important, as the care home study by Fitton et al also suggested that stand alone DNACPR forms are poorly understood by some professionals, and that in practice, DNACPR recommendations sometimes meant that other medical treatments and hospital admission were taken off the table.
Would using ReSPECT forms avoid some of the problems with variable practice and misinterpretation of DNACPR forms? Ethnographic research suggests that even ReSPECT forms are not used quite as intended to fully explore patient preferences in decision-making. Despite containing spaces for clinical recommendations for medical, emergency care and treatment, most discussions with patients focussed just on CPR.4 But this research was conducted in a hospital setting, which is a very different space where DNACPR discussions are sometimes conducted when a patient’s clinical condition is deteriorating and decisions about what to do at the end of life are more pressing.
ReSPECT in general practice
In general practice (possibly unlike many hospital circumstances) we can discuss end of life and treatment escalations decisions with patients before they become very unwell…
In general practice (possibly unlike many hospital circumstances) we can discuss end of life and treatment escalations decisions with patients before they become very unwell, and this is where the ReSPECT process could potentially give a space for a meaningful patient-centred discussion about preferences at the end of life. But how widely are ReSPECT forms used in general practice? Some (now historical) clinical commissioning groups (CCGs) adopted ReSPECT forms, but there is far from a national adoption of ReSPECT in community settings. Some regions have adopted a treatment escalation plan (TEP) form, which is a ReSPECT-light document that looks similar to the old red-bordered DNACPR forms, but includes questions about whether acute hospital admission or treatments are appropriate. Should we be using ReSPECT forms in general practice? A planned study by a Bristol-based team of researchers is looking at just that, and will examine the implementation of ReSPECT across the Bristol, North Somerset and South Gloucestershire CCG from 2019.5 This research will give us more information about how ReSPECT forms were used, and whether there were any changes in care recommendations, DNACPR decisions, and end of life outcomes in a community sample.
Research, especially in care home settings, is showing that we could be doing a lot better in talking to patients and their families about their wishes at the end of life and what ‘do not resuscitate’ means to them, discussing when hospital admission might be suitable or not, and then communicating those decisions to other healthcare professionals such as care home staff. ReSPECT forms might provide the platform to facilitate those discussions, but it’s just a piece of paper, and is only as good as the discussions we have with patients and their carers that underpin what’s written on it.
References
- Etheridge Z, Gatland E. When and how to discuss “do not resuscitate” decisions with patients. BMJ. 2015;350:h2640.
- Fitton EK, M.; Wyllie, A.; Michalowski, S.; Bhatt, V.; Martin, W. Managing DNACPR recommendations in residential care: Towards improved training for social care and capacity professionals. The British Journal of Social Work. 2023.
- Hawkes CA, Fritz Z, Deas G, Ahmedzai SH, Richardson A, Pitcher D, et al. Development of the Recommended Summary Plan for eEmergency Care and Treatment (ReSPECT). Resuscitation. 2020;148:98-107.
- Eli K, Hawkes CA, Ochieng C, Huxley CJ, Baldock C, Fortune PM, et al. Why, when and how do secondary-care clinicians have emergency care and treatment planning conversations? Qualitative findings from the ReSPECT Evaluation study. Resuscitation. 2021;162:343-50.
- McDermott A, Woodall CA, Chamberlain C, Selman L, Pocock LV. Which patients received a ReSPECT form, what was documented and what were the patient outcomes? A protocol for a retrospective observational study investigating the impact of the COVID-19 pandemic on the implementation of the ReSPECT process. BMJ Open. 2022;12(7):e060253.
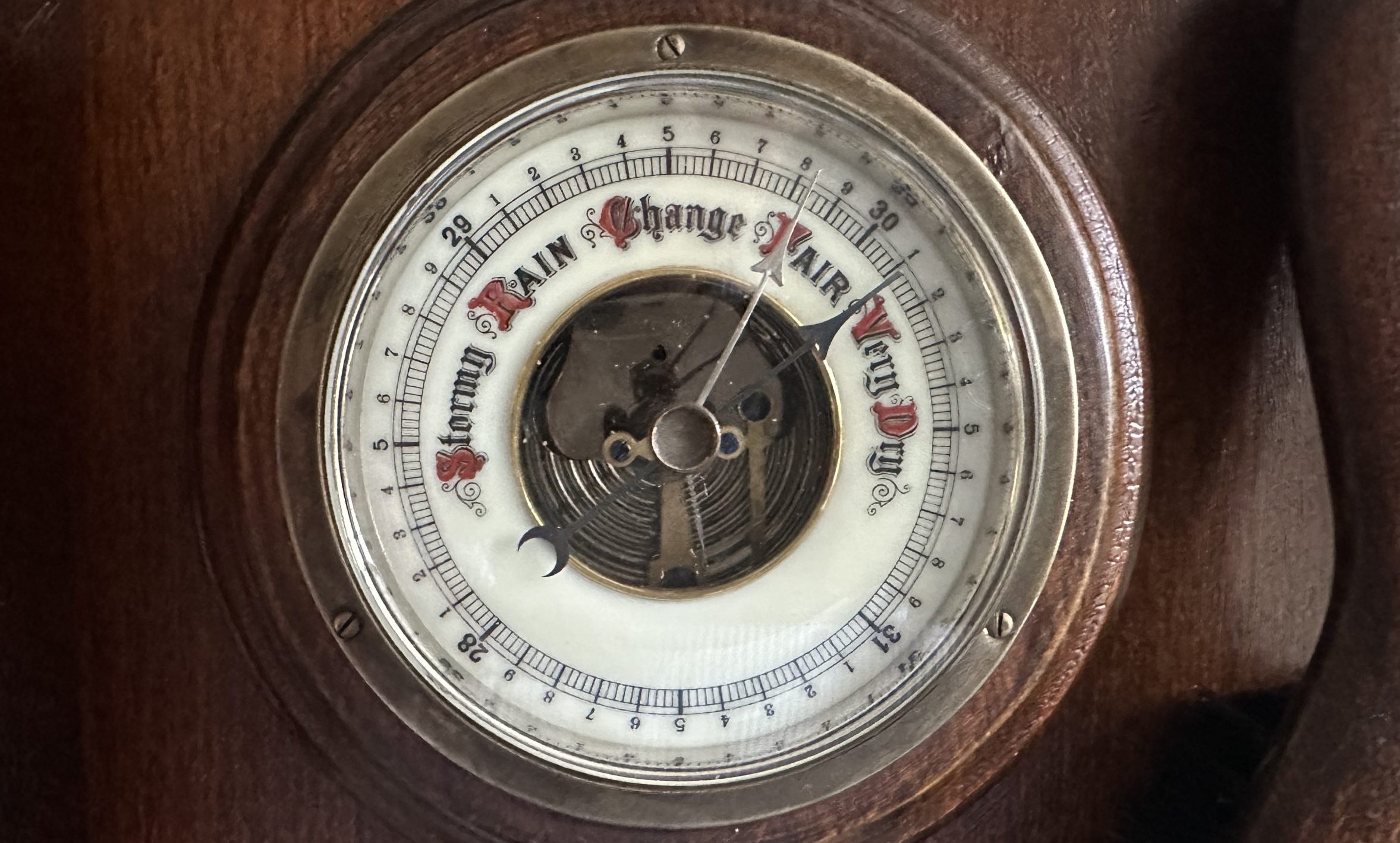
Featured photo by Danie Franco on Unsplash