
Childhood adversity or childhood trauma has been, and continues to be, connected to poor quality of health and life. A growing body of evidence points to millions of people across the world experiencing events in their childhood that are detrimental to their physical and mental development.
As a GP, I have grown to be interested in this subject and the role that primary care may have to play in mitigating the impact of this adversity. This is a complex intergenerational problem that will require many streams of solutions. What I do know is that every day patients tell me of the trauma they have experienced in their lives, be that as a child or as an adult.
This is a complex intergenerational problem that will require many streams of solutions.
Fibromyalgia and chronic pain are common diagnoses found and coded in primary care. In the UK approximately 28 million people are thought to be affected by chronic pain (CP).1 Chronic pain is a complex problem across the world, costs the UK economy millions of pounds a year and detrimentally impacts the quality of lives. Primary care manages the vast majority of patients with chronic pain whether or not there is a specific diagnosis, or it has an unknown origin. Only a small percentage of patients are referred to a secondary care pain clinic. One paper has reported that 22% of GP consultations are regarding chronic pain.2 Childhood adversities are common across the world; the average number that people experience before the age of 18 is 2.5-2.9 different types of trauma.3 Negative experiences in childhood include physical, emotional neglect and abuse, sexual abuse and family dysfunction as well as living with those with poor parental mental health or incarceration. These have been linked to chronic health conditions, including chronic pain, in adulthood.4
Childhood adversity can lead to more pain and greater dysfunction with the pain experienced. [5] There is some debate in the literature, but childhood adversity is thought to be associated with fibromyalgia with family dysfunction such as conflict, divorce and being fearful of a family member, alcohol abuse in parents being directly linked. [6] Emotional neglect, lack of affection and emotional abuse often goes unnoticed but can be linked to pain. Studies have concluded that patients with chronic pain should be asked about childhood trauma or current traumatic events. [7] Studies also show that if any childhood adversity is not identified then management plans may not be as effective[8].
For example, women with fibromyalgia may benefit from trauma focused care [9] and those with post-traumatic stress disorder arising from childhood adversity and chronic pain may benefit from therapy focusing on emotional regulation [10]. However, we will not be able to refer people for these therapies if we do not know that trauma is part of their story. Assessing for any childhood adversity can therefore be important to developing management options for their pain. More societal education on the detrimental impact of childhood adversity is required. Further larger scale research should address the assessment and management of these long-term sequelae of childhood adversity in primary care. Children should be safe in their environments at home, and for those who did not have a safe secure environment growing up and now experience pain, more consideration is required. Prevention of childhood adversity is crucial in reducing the impact chronic pain has in adulthood.
Try this in your practice: an audit
A question grew in my mind: If trauma was associated with fibromyalgia and chronic pain, were we asking about it?
A question grew in my mind: If trauma was associated with fibromyalgia and chronic pain, were we asking about it? As a result I conducted a short audit in an inner-city GP practice in Scotland. My aim was to look and see what traumatic events, in adulthood or childhood were being documented or enquired about for those who have been coded as chronic pain (CP) or fibromyalgia (FM). Literature review determined the most commonly used expressions of childhood adversity or current adversity as: abuse, trauma, neglect, adversity, or maltreatment. For the purposes of the audit the term ‘trauma’ was used to encapsulate all known terms.
The practice has a mixed demographic across areas of deprivation. The practice has 6,094 patients looked after by 5 GPs and 2 practice nurses as well as an extended team of administration staff, district nurses, health visitors and psychology clinical assistant. Patients coded with either CP or FM were identified. Using the practice-based Vision software, electronic notes were searched for the above terms to determine whether patients with these conditions had ever been asked about these negative life events. Ethical approval was not required as this was an audit based in a single practice. A total of 98 patients were identified with chronic pain, fibromyalgia and both conditions.*
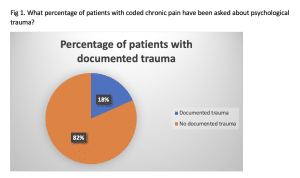
Figure 1 shows the results from across the 2 VisionTM codes utilised; CP = #1M52, FM = #N248.
The graph shows that that trauma had not been documented in many patient notes that have these codes.
Types of trauma that had been revealed and documented:
- Road Traffic Accident
- Childhood abuse
- Experience abuse as an adult
- Domestic abuse as an adult
- Physical trauma
- Witnessing traumatic event
- Sexual abuse as a child
- Sexual and physical abuse as a child
- Physical and emotional abuse as a child
- Road traffic accident
This audit shows that only small numbers of patients had had trauma documented in primary care in this practice.
*The data are reproduced with the permission of and verification by the relevant practice, which have been submitted to the editorial team
References
1. Fayaz, A., et al., Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open. 2016 Jun 20; 6 (6): e010364. doi: 10.1136/bmjopen-2015-010364.
2. Mills, S., N. Torrance, and B.H. Smith, Identification and Management of Chronic Pain in Primary Care: a Review. Curr Psychiatry Rep, 2016. 18(2): p. 22.
3. Kessler, R.C., et al., Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. The British journal of psychiatry, 2010. 197(5): p. 378-385.
4. Felitti, V.J., et al., Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine, 1998. 14(4): p. 245-258.
5. Brown, R.C., et al., Associations of adverse childhood experiences and bullying on physical pain in the general population of Germany. J Pain Res, 2018. 11: p. 3099-3108.
6. Varinen, A., et al., The relationship between childhood adversities and fibromyalgia in the general population. J Psychosom Res, 2017. 99: p. 137-142.
7. Gunduz, N., et al., Psychiatric comorbidity and childhood trauma in fibromyalgia syndrome. Turkish Journal of Physical Medicine and Rehabilitation, 2018. 64(2): p. 91-99.
8. Hart-Johnson, T. and C.R. Green, The impact of sexual or physical abuse history on pain-related outcomes among blacks and whites with chronic pain: gender influence. Pain Med, 2012. 13(2): p. 229-42.
9. Gerber, M.R., et al., Experience of Childhood Abuse and Military Sexual Trauma Among Women Veterans with Fibromyalgia. J Gen Intern Med, 2018. 33(12): p. 2030-2031.
10. Powers, A., et al., Childhood abuse and the experience of pain in adulthood: the mediating effects of PTSD and emotion dysregulation on pain levels and pain-related functional impairment. Psychosomatics, 2014. 55(5): p. 491-499.
Featured image by Adrian Swancar on Unsplash







Karen – I loved reading your article on fibromyalgia and chronic pain. I am a GP in Somerset with a similar interest in how we integrate the science of how adversity affects human physiology into Primary Care. I have written a coaching programme which is being accessed by workers from across health, education and care who are looking for different ways of working that enable these difficult conversations with patients using a coaching style. In order to be able to ‘sit with’ patients as they process their reality we first need to develop insight into our own emotion responses and emotion regulation. http://www.alpiricoaching.co.uk
Scott Wylie is a 3rd year medical student at the University of Glasgow. Paul McNamara is a GP in Glasgow and honorary clinical lecturer at…
[…] https://bjgplife.com/fibromyalgia-and-chronic-pain-are-we-asking-about-psychological-trauma-or-traum… […]