 Sinead Millwood is a salaried GP working for Hope Citadel, a community interest company in Manchester running GP practices in areas of deprivation. She is passionate about campaigning for clean air, primary care research, and women’s health. Bernadette Millwood is a Co-Clinical Director of Icknield PCN in Hertfordshire. She has now retired as Lead GP Nurse at the Baldock Surgery where she had a special interest in respiratory. She is retiring from her role as CD at the end of February 2024.
Sinead Millwood is a salaried GP working for Hope Citadel, a community interest company in Manchester running GP practices in areas of deprivation. She is passionate about campaigning for clean air, primary care research, and women’s health. Bernadette Millwood is a Co-Clinical Director of Icknield PCN in Hertfordshire. She has now retired as Lead GP Nurse at the Baldock Surgery where she had a special interest in respiratory. She is retiring from her role as CD at the end of February 2024.
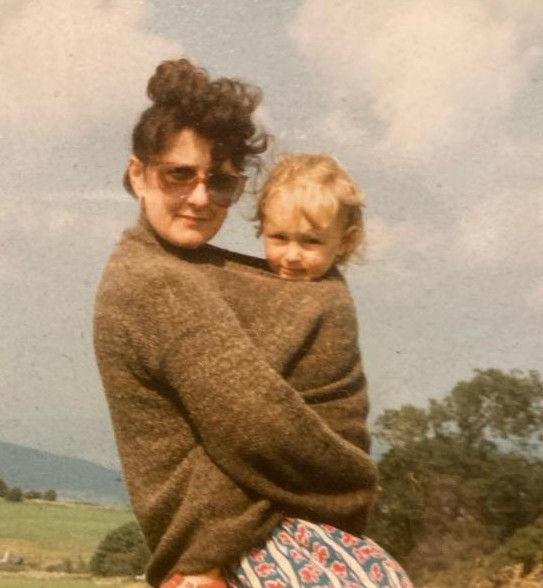
Some of my earliest memories are mum picking me up from school. ‘Who is that in the uniform?’ my classmates would say. ‘That’s MY mum. She is a nurse!’ The pride I felt as a child in her vocation was powerful, but naive. Only now that I’m a GP do I understand the true magnitude of her achievements in her 44-year career.
She completed training at Birmingham School of Nursing in 1979, worked in intensive care units for 6 years, and later as a research nurse for GlaxoSmithKline and as a community nurse, making the move to general practice in 1993. More recently she has taken leadership roles as primary care nurse tutor and Co-Clinical Director (CD) of her Primary Care Network (PCN), one of only 14 nurse CDs in the UK.
Retaining your practice nurse
Nursing in the UK is in crisis with the current argument over pay and working conditions, and record numbers leaving the profession. Data from NHS England show some 47 496 vacancies. I asked mum why nursing is not as attractive as it was.
‘Practice nurses are feeling very undervalued, there’s no doubt about it. They’re not Agenda for Change. All staff employed by the Additional Roles Reimbursement Scheme (ARRS) are Agenda for Change, which means that all of them get a certain level of pay, which is probably higher than the practice nurse. They have a lot of holiday and practice nurses don’t get that, they get whatever they’ve negotiated.’ In addition, there seems to be a feeling of a general lack of appreciation.
Nursing in the UK is in crisis with the current argument over pay and working conditions, and record numbers leaving the profession. Data from NHS England show some 47 496 vacancies.
‘I know of nurses who have come in and worked during booked annual leave. If somebody has the decency to do that, you have to reward them. You can’t just say, “Oh, thanks.” You have to say, “Wow, that was brilliant of you, thank you so much for coming in, now take your week off.” But no one says that and the nurse feels undervalued and ends up leaving.’
Practice managers and lead GPs can support nurses by respecting their professional autonomy
‘If I feel that somebody needs a double appointment I can book a double appointment. That doesn’t happen in all practices and it can be undermining. A professional should be able to use their initiative and experience to determine a safe course of treatment for a patient.
‘Well obviously I’ve stayed for twenty-nine years. When doctors and practice managers have asked me why a nurse is leaving I say, “You never ask the people who stay why they stayed. Nobody’s ever asked me.”
‘I stayed because I’m respected and listened to. I do the training that I believe will benefit the practice.’
‘I stayed because I’m respected and listened to. I do the training that I believe will benefit the practice. My surgery has always had a flexible approach to working hours, to me that was very valuable. All those things add up to I’m happier and more fulfilled here than going somewhere else.’
GP wellbeing
Throughout her career, mum has seen GPs and nurses come and go. I asked her what the attributes were that have enabled her longest working colleagues to continue.
‘It’s teamwork. In my experience in our practice, when doctors are under pressure they tend to isolate themselves. It’s important to make sure everybody’s OK and show that you care about your colleagues, just check up on them.’
Mum has a seemingly simple tip for improving wellbeing at work.
‘In my experience in our practice, when doctors are under pressure they tend to isolate themselves. It’s important to make sure everybody’s OK and show that you care about your colleagues …’
‘When I took over as team leader, I said I’m not having thirty minutes’ lunch, I’m having an hour. I don’t care if half an hour is unpaid. In that hour we have really healthy food and sit and reflect on the morning’s work. A lot of other surgeries make the nurses go to lunch on their own and you’re already isolated in general practice. We often sit with the receptionists as well. They listen to us and we listen to them. Little tiny glitches can be sorted out in those lunchtime meetings. We know it’s precious and we hang on to it.’
The GP–nurse relationship
I wondered how the relationship between nurses and doctors has changed over her career.
‘Years ago a friend of mine was doing midwifery training, there was a consultant there, who whenever he examined a woman internally, afterwards he used to put his hand up in the air, and the sister took his glove off for him. He couldn’t quite remove his own glove! So we have made some progress.
‘When my sister went into nursing in the sixties she wore a starched apron and a little hat, well that’s a maid isn’t it?! I mean when I came to London, as an agency nurse at Saint Thomas’, the nurses were called Blue Belt Frillies and Pinks. They had to get away from that because nurses are professionals. I think it was only in Project 2000 when nursing became a degree course that they started to be seen as professionals. But even now if you stand a nurse who’s got a degree next to a pharmacist who has a degree, I don’t think it’s seen as quite the same. It seems less studious because it’s a caring profession.
‘When I started in general practice there was still a hierarchy issue, but I think because I’ve worked there for so long, I have a different relationship with the doctors now than I did. Our current GPs have a much more collaborative approach. They do respect the nurses that have been there a long time. Though respect seems to need to be earned by nurses. It is not immediate.’
This need to earn respect for new nurses is in stark contrast to my experience as a new doctor on the receiving end of what feels like undeserved respect from nursing colleagues. Often older and much more experienced than me. I think a lot of young doctors feel awkward about this undue deference.
‘Our current GPs have a much more collaborative approach. They do respect the nurses that have been there a long time.’
‘That’s how they were trained and they may have been patronised by doctors in the past. I think if doctors and nurses were interacting on a training level, things would be different. There’s no reason why nurses and doctors can’t do modules in overlapping skills, like prescribing or phlebotomy, together. But it’s all very separate. Nurses and pharmacists do some modules together, but not doctors.’
General practice has changed
GPs are having the same workforce challenge as nurses, with numbers of GPs at a 30-year low.
‘I think that the partnership model is in danger. It’s a huge commitment to be a partner. The role is so much more than it was. They employed practice managers, but now you often have a business manager as well. So even that job is too big.
‘My observation is that being a GP is really hard at the present time. Mainly because now patients have multiple problems. Also, the work is never ending. Now you have tasks, emails, instant messaging, scans, lab results, you still have a physical tray to look through daily. You’re going from one thing to another. It’s just too many ways of communicating all at the same time. We go home sometimes and the partners are still there at eight, nine o’clock at night.
‘When I started practice nursing we did split shifts, I mean doctors used to go and play golf in the middle of the day and then go back and do an evening surgery. Well, there’s no such thing as evening surgery now. It’s all one long day, isn’t it? That’s the problem. It’s all merged. I think practices need to be just a bit more flexible in their working patterns.’
‘… being a GP is really hard at the present time … the work is never ending. Now you have tasks, emails, instant messaging, scans, lab results, you still have a physical tray to look through daily.’
As a GP my concern about moving away from the partner model would be ensuring that strong clinical leadership, and not business leaders, are making decisions about patient care.
Nurse Clinical Director
Mum was put forward for the CD role by a GP colleague, a role she shares with a GP. As one of the few nurse CDs in the UK, I asked mum what value nurses bring to a role that’s currently usually occupied by GPs.
‘We know the whole workforce. I think the GPs know the GPs, and I know everybody else, all the healthcare assistants and practice nurses and the additional roles. It’s all about forming good working relationships. I think operationally nurses are pretty good at instigating and setting up systems.’
As a CD, mum has been involved in commissioning new services and additional roles for her PCN. I wondered what have been their biggest successes?
‘COVID happened six months into PCNs. They were crazy times and all of a sudden we had to set up vaccination centres. So working with a doctor and a nurse, it worked out very well and I’m very proud of the job we did. All the doctors and nurses from the six practices worked together. There was a strong feeling of camaraderie created during COVID which we are now building on.
‘The biggest success we’ve had with additional roles is the pharmacy team. We now have one pharmacist per practice and they have started to do their prescribing courses. We also have a pharmacist looking after the care homes so we feel that was a big step forward because we have nine care homes and that is a lot of work taken off the practices.’
‘I think the traditional model was struggling … it’s got to change. Collaborative working is the only way forward.’
The creation of PCNs is changing the face of general practice in the UK, but has it been for the better?
‘I think it had to happen, because I think the traditional model was struggling. We have been working within this model since 1948, it’s got to change. Collaborative working is the only way forward.’
What we should learn from my mum
In a world where GPs are working on their laptops into the night after a full day of work, often without a conversation with a single colleague, we continue to think we can carry on alone. The days of playing golf at lunch are so over we often no longer take lunch, and the job is becoming so unmanageable we are haemorrhaging colleagues to early retirement and burnout. I know of two of my own training cohort who have already made a sideways move into sexual health and palliative care after only a year in the job. Simple but seemingly impossible culture changes, like having an hour for lunch with colleagues, like feeling you can ask for help, like knowing the practice manager will respect and consult your clinical opinion before making decisions, could make all the difference. Naively I had thought that my generation of doctors viewed nurses as equals. When a dinosaur cardiologist disparaged nurses in his speech at our medical school halfway ball, he received a boo. But though we do seem to have learned how to take off our own gloves, we still don’t value our practice nurses as we should. Mum feels guilty for being paid so much as a CD, but it’s clear to me they have got themselves a bargain. A bargain every PCN and GP practice could benefit from if we invest in our nurses, train them as far as they want to go, advocate for them as my mum’s GP colleague has done for her, pay them what a professional with a degree should be paid. Stop taking their commitment and hard work for granted and learn to say thank you. Respect them enough to give them autonomy over their appointments and listen to their ideas. Then, maybe, there will be more highly qualified nurses like my mum, who could successfully work with GPs to take on CD roles and share the task of improving primary care in the UK.
… there will be more highly qualified nurses like my mum, who could successfully work with GPs to take on CD roles and share the task of improving primary care in the UK.
‘You’ve got to have more nurses in there or pharmacists or somebody else other than GPs. It’s about the whole primary care network team. You need to listen to different viewpoints. NHS England have made the decision to bring in other professions so other professions have to have a say in the future of primary care.’






It made me weepy reading this dose of common sense, knowing that my sister-in-law and niece were taking the trouble to communicate so clearly what has been a huge contribution to successful and effective practice. Working with your hands has forever been looked down on, whether industry or public service. Such ignorance of the intelligence, knowledge and experience that such work demands is widespread – in education and society. Thanks both for taking on the service you have and making this so clear!
Very well said, very interesting