On 29 November 2025, I visited an installation created by the artist, Charlotte Mann. For a few short weeks, before the house was sold, Charlotte curated an exhibition that summarised an exceptional family in their home, 179 Burnt Ash Hill, SE12. The three ‘practices’ of medicine, law, and art together in three generations.
Charlotte’s grandfather, Charles Carey (Charlie), purchased the house in 1945 and had a doctor’s surgery built onto the side. From there until 1979/1980 he practiced medicine as a local GP in suburban South London. In common with many GPs up and down the country, he saw his patients, did house calls, and was the centre of local life.
The practice
“In common with many GPs up and down the country, he saw his patients, did house calls, and was the centre of local life.”
I got off the train and walked the 20 minutes up from Lee station to the house, which was up a hill with sweeping views down across the rest of London towards Bromley and Kent. I walked up the garden path. The sign said: ‘Morning surgery 9–10:30 Evening 5:30–7. No evening surgery Thursday and Saturday.’
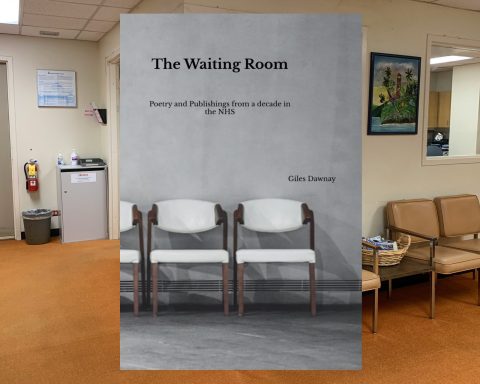
This was a sit-and-wait operation, as so many GP surgeries were for decades. No computers, just the cardboard pouches of Lloyd George notes in their little drawers in the reception. There was not always a receptionist. There was a line of chairs in the waiting room, and the patients simply moved up the line until it was their turn. So simple, and yet so effective. I remember when I started as a partner 20 years ago, a particular group of patients were not pleased when they discovered their special ‘jumping the queue chair’ had been done away with, as I felt patients should be seen in turn.
Along the side of the waiting room was a typical but small glassed reception area with Charlotte’s daughter, Zoe, there to greet me, take my details, and give me a ‘prescription’. Inside the reception area were the many drawers for the Lloyd George records. The Careys didn’t believe in throwing things away and continually buying new things — they believed in continuity and loving objects that worked for them. The drawers had evidence of being loved, with handles replaced and mended, and regular maintenance.
As in any GP practices, there were information leaflets on a small table and posters up around the waiting area. ‘Problems with the cold? Ring the Freeze Phone’ leaflets for patients on gout, lumbar disc disorders, and rheumatic fever printed by the Arthritis and Rheumatic Council (now Versus Arthritis) were all very familiar. Many of my patients still want things printed out and are not happy when offered a link on a text message. What especially tickled me was ‘If you MUST ask the doctor to call, please phone before 10 am.’

The patient list
In 1959, according to a notice from the ‘Distribution of Practitioners Fund’, Charlie had 417 patients on his list for General Medical Services (GMS) and three temporary patients. By 1973, a similar typed notice declared he had 437 ‘ordinary’ patients for GMS and 51 ‘elderly’ — making a total of 488. An early form of weighting the population. Imagine the care GPs could provide nowadays with those numbers!
I thought of the privilege being a GP has given me. That people are willing to share their inner-most secrets. One of the joys of our work is meeting patients again and again, and remembering the life experiences that have shaped them over the years. I think about how intimately I would know my 488 patients.
Through the waiting room led to the one-room GP surgery. Charlie sat at a small bureau desk (no room for a computer), with compartments for sick notes, maternity certificates (‘certificates of confinement’), and prescriptions. The MIMS (Monthly Index of Medical Specialities) annual compendium lay open. Some equipment lay around — blood pressure machine on the wall — and the couch.
“One of the joys of our work is meeting patients again and again, and remembering the life experiences that have shaped them over the years.”
A notice on the wall explained that ‘under the sheet that the patient sat on Charlie placed a blanket that he had saved from D-day when working on a hospital ship. He had spent a long time saving the life of a German solider. This was the blanket that had been wrapped around that young man.’ I wondered what the infection control team would say about this nowadays, and the impact this experience could have had on Charlie as he looked after his patients.
Some things were so familiar — a photocopy of ‘the limited list’ was stuck to the wall with Sellotape. In 1985, the government restricted the range of certain medications that doctors could prescribe on the NHS. The goal was to reduce rising pharmaceutical expenditure. It was highly controversial at the time but only the start of ongoing infiltrative government involvement with GP prescribing.
Charlie’s typical day in the 1960s involved surgery 9–12 am — no appointment, no receptionist; 12–1 pm — home visits — then picked up Frances (Charlotte’s mother) from school and they came home for lunch made by Nanna; 2–5 pm — more calls and home visits; 5–6 pm — tea — a pile of hot buttered toast made by Nanna; and 6–9 pm evening surgery. The household had dinner at 8 pm and he would join when he was finished; 10–11 pm — paperwork in surgery. What a relentless schedule. But what a level of care his patients must have received. The evening surgery was brought earlier as time went on.
I spent some time taking in the space. Imagining the consultations and interactions that had taken place there for nearly 40 years. Charlie was a well thought of local GP and clearly trusted by patients. Charlotte has written: ‘When Charlie’s son, Patrick, was studying medicine, he asked his father for advice on how to be a good doctor. Charlie’s reply was: “When someone gets up to leave the consulting room, pay attention closely to the way they grasp the door handle. If they seem at all hesitant ask them if there is anything else on their mind — it is often what I hear in this moment that makes the most difference in my being able to help them.”’
As Polly Morland says in A Fortunate Woman: ‘where the scalpel is the essential instrument of the surgeon, so the relationship is the instrument of the general practitioner … summoning afresh, in each ten-minute increment, empathy, precision, collaborative decision making and shrewd risk management.’ 1
“Being the local doctor was a 24/7 enterprise and switching off wasn’t really an option without sharing cover or arranging locums.”
Being the local doctor was a 24/7 enterprise and switching off wasn’t really an option without sharing cover or arranging locums. It reminded me of the level of availability my grandfather, who was a vicar, always had and the duty of being there for parishioners throughout their lives — including the most joyous and most sorrowful.
But this level of availability and inability to switch off takes its toll. Charlie went on a home visit one night and had a heart attack at the patient’s house. Movingly, one room in the house — Charlie’s bedroom — displays messages from all the get-well cards he received while recovering, which were all kept.
In 1986, the surgery closed its doors and the practice moved into a modern health centre nearby. Undoubtedly, working in an environment with more than one GP around to share the load would have been welcome, but I was also left thinking about what was lost.
The essence of a GP
Visiting 179 Burnt Ash Hill surgery was an important reminder to me of the essence of being a GP. What little in the way of equipment and space is really needed to carry out our craft. The magic of what happens between two humans in a room together — to elicit a solution to a problem that may or may not be pathological but needs unburdening, sharing, and puzzling out. Building this relationship over time is life-saving.2 Being able to respond to patients on both an emotional and intellectual level is what makes us GPs.
We are pushed and moulded into being ever more efficient triage bots, pigeon-holing patients via online algorithm. Artificial intelligence is deciding who gets to see the GP. It is easy to see how complex patients with a lot going on get lost among messages about ‘right care, right place, right time’ and potentially give up altogether.
A system that allows space for this life-saving relationship to develop is undoubtedly the most efficient, but this space is being crowded out. I am left wondering about the missed opportunities from our regulatory systems to put the human dimension of care front and centre,3 and what Charlie would have thought about where we have got ourselves. I left with more determination than ever to cherish these important relationships every day.
General Practice 179 was an installation by Charlotte Mann presented over November and December 2025. Due to increased demand, Charlotte will be reopening the exhibition for one extra day on Sunday 4 January from 1–4 pm. In addition, on Wednesday 7 January there will be an open evening and in-conversation event at the house. For more details please visit Charlotte’s Instagram: https://www.instagram.com/general_practice_179. For more of Charlotte’s work, please visit: https://charlottemann.co.uk.
Competing interests
The author went to primary school wth the artist, Charlotte Mann.
References
1. Morland P. A fortunate woman: a country doctor’s story. London: Picador, 2022.
2. Sandvik H, Hetlevik Ø, Blinkenberg J, Hunskaar S. Continuity in general practice as predictor of mortality, acute hospitalisation, and use of out-of-hours care: a registry-based observational study in Norway. Br J Gen Pract 2022; DOI: https://doi.org/10.3399/BJGP.2021.0340.
3. Shah R, Foell J. Fighting for the soul of general practice: the algorithm will see you now. Bristol: Intellect, 2024.
Featured photo: Reception area of the GP practice at 179 Burnt Ash Hill. Part of Charlotte Mann’s exhibition, General Practice 179. Photo courtesy of Charlotte Mann.