Stevie Lewis is a campaigner and researcher working nationally and internationally to help governments, prescribers, and patients recognise and support people with antidepressant withdrawal; a board member of the International Institute for Psychiatric Drug Withdrawal; and a member of LEAP for PDD — the Lived Experience Advisory Panel for Prescribed Drug Dependence.
Mark Horowitz is a Clinical Research Fellow in Psychiatry at North East London NHS Foundation Trust; an Honorary Clinical Research Fellow at University College London; and a training psychiatrist with a PhD from the Institute of Psychiatry, Psychology and Neuroscience at King’s College London in the neurobiology of depression and antidepressant action. Mark runs a deprescribing clinic in the NHS to help patients safely reduce and come off their antidepressants.
Most people, including doctors, believe that it is not difficult to stop taking an antidepressant and that this can be completed over a few weeks.1 The reality is that some people experience difficult, and in some instances debilitating, withdrawal effects.2
Patients often report that their withdrawal symptoms are misdiagnosed as a return of an underlying condition,3 likely because doctors have had little training on the recognition of withdrawal symptoms.
There has been long-standing minimisation of the extent and severity of withdrawal, with the National Institute for Health and Care Excellence (NICE) guidelines describing them as ‘usually mild and self-limiting’ for many years.4 This guidance was informed by studies performed by drug manufacturers for people who had been on the drugs only a few weeks, but is now recognised not to be accurate for people who have been on them for months or years,5 as many patients are.
“… over half of people taking an antidepressant will experience some form of withdrawal when they reduce or stop … “
The new NICE guidance on depression6 includes an update on the severity of withdrawal symptoms and a dedicated section on how to safely stop antidepressants (pages 18–21). It also links to the Royal College of Psychiatrists guidance on stopping antidepressants as an educational resource.7
There are myriad withdrawal symptoms because the neurotransmitters in the brain affected by antidepressants, including serotonin, among others, affect many different bodily systems. Physical symptoms include dizziness, sensory problems such as vertigo, increased sensitivity to light and sound, and electric shocks in the head known as ‘brain zaps’; muscle problems like tremors, spasms, and trouble with coordination; and sometimes akathisia, a feeling of agitation and inner restlessness that is so unpleasant some people feel suicidal.
Psychological and emotional symptoms include crying, depression, panic attacks, and anxiety so bad some people describe it as terror. Given these symptoms overlap with mental health conditions it is easy to understand why doctors might jump to the conclusion that they are seeing a return of an underlying mental health condition.
Distinguishing withdrawal from relapse can be difficult.3 As we now know that over half of people taking an antidepressant will experience some form of withdrawal when they reduce or stop,5,8 doctors should have a high index of suspicion for withdrawal.
Withdrawal symptoms tend to come on soon after reducing or stopping medication — often days — quicker than a relapse would occur; although we know that in some people withdrawal symptoms can be delayed. The presence of physical symptoms — dizziness, headache, and brain zaps — along with emotional symptoms can help mark it out as withdrawal. Reintroducing the drug often causes withdrawal symptoms to resolve quickly.
“Withdrawal symptoms are not a sign that a patient needs the drug, but a sign that they need to reduce the drug more slowly.”
Withdrawal symptoms are not a sign that a patient needs the drug, but a sign that they need to reduce the drug more slowly. It is also important for doctors to recognise that antidepressant withdrawal can sometimes be severe and long-lasting (as long as months or even years), more likely for long-term users. This is down to the profound, slow-resolving changes to the brain caused by these medications.5
To minimise withdrawal effects, first, tapering must be done gradually: this often involves tapering over months, or even years, especially if the drug has been taken for long periods — and not weeks. This allows the brain to adapt to the changes. Stopping these drugs too quickly is a bit like jumping off the tenth floor of a building in terms of the changes the brain is asked to cope with. Coming down step by step over a longer period of time causes much less disruption to the system.
Second, the rate must be adjusted to the individual. Everyone is different so it is hard to determine ahead of time. The best way to work this out is through a test reduction to see how someone responds to determine further steps.
Lastly, extra care must be taken on reaching the last few milligrams of the drug. This is because very small doses have much larger effects than one would expect, as seen in nuclear imaging of the effect of antidepressants on target receptors (Figure 1).9 The law of mass action applies: when there is little drug about every extra milligram has a large effect, but when it is more crowded with drug every extra milligram has less and less additive effect. An example of the law of diminishing returns. For example, 2 mg of a drug (a seemingly tiny amount) often has about half the effect of 20 mg of the drug (Figure 1).
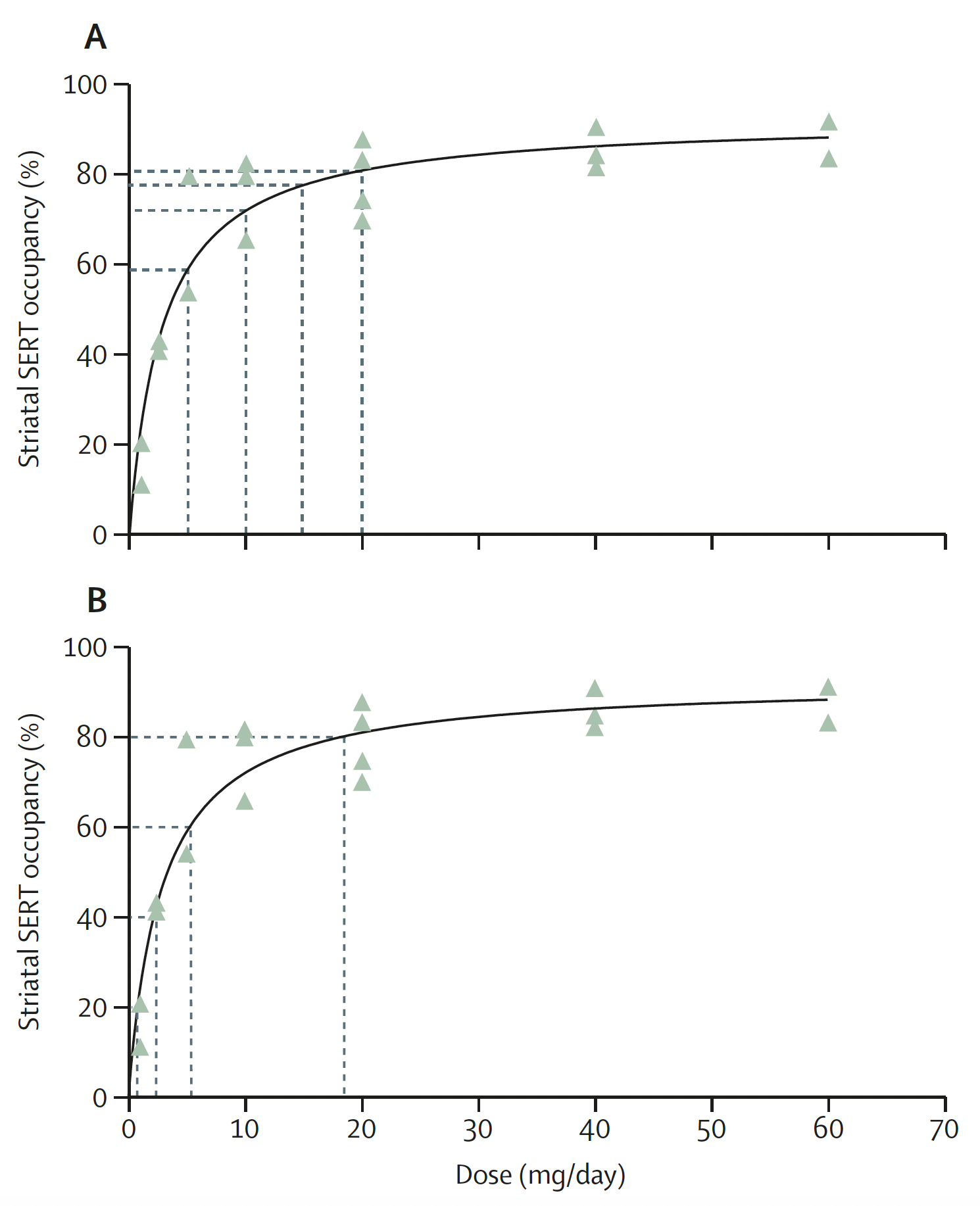
This means reductions must be made very slowly at lower doses. In linear tapering — currently, the most common approach — the final reduction from 5 mg to 0 mg causes a huge change in effect on the brain (analogous to jumping from the seventh floor to the bottom) (Figure 1). On the other hand, reducing the dose more carefully at the end — called hyperbolic tapering, because this shape is a hyperbola — means that you make a soft landing at the end (walking down the steps all the way to the bottom). This approach is currently recommended by NICE and can allow many people to be able to safely stop their antidepressants, who could not with a linear approach.
Competing interests
Mark Horowitz is a collaborating investigator on the National Health and Medical Research Council and Medical Research Future Fund-funded RELEASE and RELEASE+ trials in Australia investigating supported, hyperbolic tapering of antidepressants. He is a co-founder of Outro Health, a digital clinic helping people to safely stop no longer needed antidepressant medication in North America using supported, hyperbolic tapering. He has received honoraria for lectures on deprescribing from NHS Trusts, Washington University, and the University of Arizona.
References
1. Read J, Moncrieff J, Horowitz MA. Designing withdrawal support services for antidepressant users: patients’ views on existing services and what they really need. J Psychiatr Res 2023; 161: 298–306.
2. Guy A, Brown M, Lewis S, Horowitz MA. The ‘patient voice’: patients who experience antidepressant withdrawal symptoms are often dismissed, or misdiagnosed with relapse, or a new medical condition. Ther Adv Psychopharmacol 2020; 10: 2045125320967183.
3. Horowitz MA, Taylor D. Distinguishing relapse from antidepressant withdrawal: clinical practice and antidepressant discontinuation studies. BJPsych Advances 2022; 28(5): 297–311.
4. Iacobucci G. NICE updates antidepressant guidelines to reflect severity and length of withdrawal symptoms. BMJ 2019; 367: l6103.
5. Horowitz MA, Framer A, Hengartner MP, et al. Estimating risk of antidepressant withdrawal from a review of published data. CNS Drugs 2023; 37(2): 143–157.
6. NICE. Depression in adults: treatment and management. NG222. 2022. https://www.nice.org.uk/guidance/ng222 (accessed 8 Sep 2023).
7. Royal College of Psychiatrists. Stopping antidepressants. 2020. https://www.rcpsych.ac.uk/mental-health/treatments-and-wellbeing/stopping-antidepressants (accessed 14 Sep 2023).
8. Davies J, Read J. A systematic review into the incidence, severity and duration of antidepressant withdrawal effects: are guidelines evidence-based? Addict Behav 2019; 97: 111–121.
9. Horowitz MA, Taylor D. Tapering of SSRI treatment to mitigate withdrawal symptoms. Lancet Psychiatry 2019; 6(6): 538–546.
Featured photo by Maksym Ostrozhynskyy on Unsplash.