Annabelle Machin is a portfolio GP working as an intern on the WiseGP programme (@wisegpcouk). She is on Twitter: @drannabellerose
James Bennett is an academic GP working in Yorkshire.
Joanne Reeve is a GP, Professor of Primary Care, and leads the WiseGP programme. She is on Twitter: @joannelreeve
Lazarus is using WiseGP resources to support mid-career GPs in reclaiming general practice
‘More of the same won’t fix general practice.’ So, what should we be doing differently? The Lazarus project is designed to take GPs out of ‘usual care’ to a different space for professional practice. In our pilot, we are prioritising a group most in need of support for something different — the burning out of mid-career GPs. Here we consider how this might help us to reclaim general practice.
Introducing Lazarus
In a service where demand exceeds supply, most ideas for change focus on improving efficiency and capacity for delivering care — trying to give GPs less work to do by introducing new technology or people to deliver ‘more of the same’.
Instead, Lazarus proposes to give GPs different work to do, work that is focused on remotivating and energising clinicians to reclaim general practice. Optimising healthcare needs to recognise both parties in the healthcare partnership, and that means supporting clinicians as well as patients.
Workforce development schemes frequently focus on GPs at the start and end of their careers, providing opportunities for development of extended professional roles to enhance recruitment and retention.1,2 Mid-career GPs are often overlooked, despite their crucial role in holding the service together, so we have started with this group.
Lazarus workshops
Lazarus workshops are a pilot for a new model of practice, designed to provide spaces for GPs to work together to develop the knowledge-in-context needed for everyday advanced generalist practice.3 So far, we’ve held 3 workshops (Figure 1).
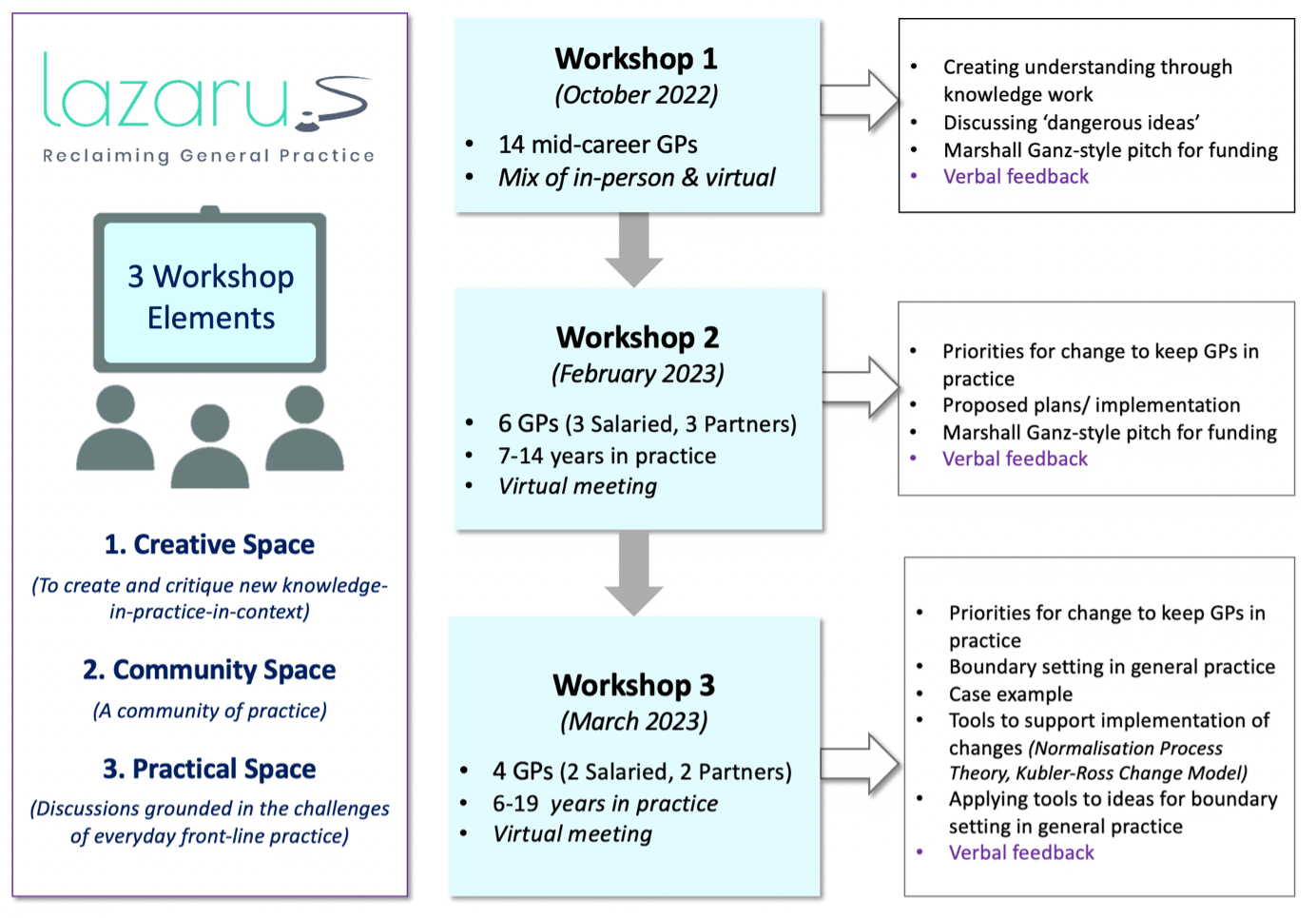
The first brought GPs together to explore their dangerous ideas4 for advanced generalist solutions (beyond guidelines) to problems faced in everyday practice. This workshop supported findings from previous work that these activities need communities to gather for facilitated professional creative activity to generate new understanding and knowledge for everyday practice.5–7
During the second workshop, GPs proposed ideas to implement to make their workloads more sustainable. Responding to feedback, the third workshop involved more-focused discussions with tangible take-home points, including tools for implementation.8,9
What did we learn from the pilots?
GPs were enthusiastic about an opportunity to shift from service delivery to being actively involved in shaping the service. They recognised that time for this work should be funded and backfilled. Many reflected how their everyday work had become isolated, so they felt workshops would provide a key space to develop a community of professional practice.
“Mid-career GPs are often overlooked, despite their crucial role in holding the service together … “
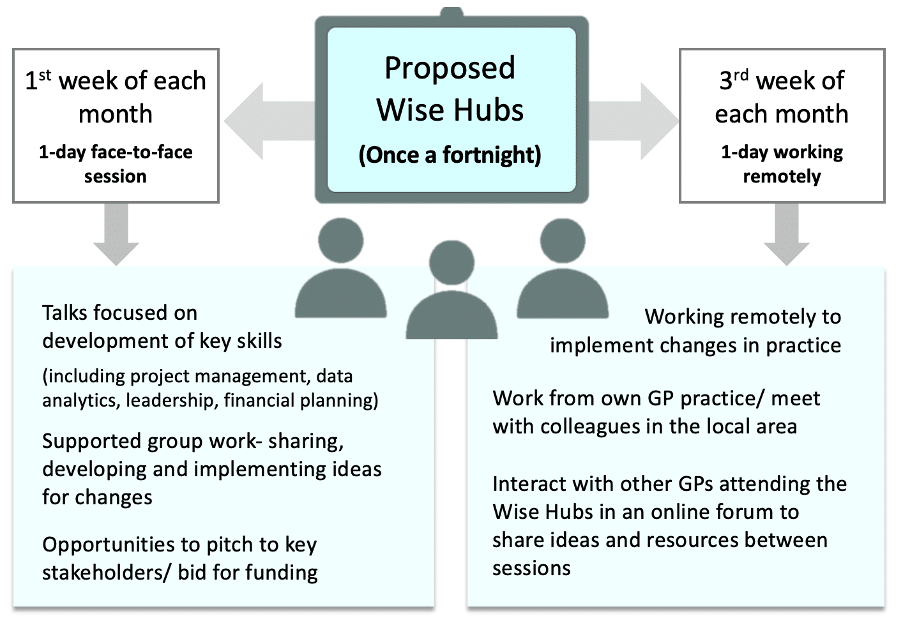
GPs were keen for inclusion of opportunities to develop their skills in leadership, data analysis, and financial planning. They felt access to stakeholders at certain workshops would help them to secure financial support for implementation of changes. Crucially, they believed involvement in this work would re-energise and retain mid-career GPs in practice.
Are Wise Hubs the future?
Two learning points from Lazarus stand out. First, rather than focusing on delivering more of the same, we need to facilitate creative activities — to develop new ways of working that support the challenges of modern practice.
Second, we need to build and support new communities of practice10 — ensuring they reflect our current multi-professional teams. To achieve this, we need protected, funded time integrated into the everyday work of all GPs,11 not bolted on as an additional, self-funded activity.
One suggestion is to rethink our funded continuing professional development activities, which traditionally involve us updating our clinical knowledge. We propose using this time even more productively, to move beyond knowledge acquisition to creating and applying the new knowledge-in-context needed to address the everyday problems we face in practice.
The Lazarus workshops suggest that our focus should not solely be on passing work to others to increase the capacity of GPs to deal with more complex problems. Instead, we can ‘protect’ mid-career GPs from workload burnout by creating facilitated, funded time out-of-practice, where they can develop and apply new initiatives that ultimately provide greater benefits to staff, patients, and the wider NHS. This is the culture shift called for by Fuller.12
We are aiming to create Wise Hubs11 to enable this practice. Here, mid-career GPs would have the time and headspace to tackle problems, generating new ways of working for everyday practice (see potential model in Figure 2).3
Do you think this work could help us reclaim general practice? Let us know your thoughts at WiseGP and on Twitter!
References
1. Leicester, Leicestershire and Rutland Training Hub. First 5 training hub. https://www.llrtraininghub.co.uk/first5 (accessed 28 Jun 2023).
2. NHS England. National GP Retention Scheme. https://www.england.nhs.uk/gp/the-best-place-to-work/retaining-the-current-medical-workforce/retained-doctors (accessed 27 Jun 2023).
3. Reeve J. “More of the same won’t fix general practice”. BJGP Life 2023; 17 Jun: https://bjgplife.com/more-of-the-same-wont-fix-general-practice (accessed 27 Jun 2023).
4. Reeve J. The SAPC Dangerous Ideas Soapbox. 2016. https://sapc.ac.uk/article/sapc-dangerous-ideas-soapbox (accessed 27 Jun 2023).
5. Gabbay J, le May A. Mindlines: making sense of evidence in practice. Br J Gen Pract 2016; DOI: https://doi.org/10.3399/bjgp16X686221.
6. Bansal A, Greenley S, Mitchell C, et al. Optimising planned medical education strategies to develop learners’ person-centredness: a realist review. Med Educ 2022; 56(5): 489–503.
7. Hull York Medical School. GP training: CATALYST. https://www.hyms.ac.uk/continuing-education/catalyst (accessed 27 Jun 2023).
8. Murray E, Treweek S, Pope C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010; 8: 63.
9. Buehring S. Kubler Ross change curve. 2021. https://www.knowledgetrain.co.uk/change-management/change-management-courses/change-management-models/kubler-ross-change-curve (accessed 27 Jun 2023).
10. Gabbay J, le May A. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ 2004; 329(7473): 1013.
11. Reeve J. Medical Generalism, Now! Reclaiming the Knowledge Work of Modern Practice. Boca Raton, FL: CRC Press, 2023.
12. Fuller C. Next steps for integrating primary care: Fuller stocktake report. 2022. https://www.england.nhs.uk/wp-content/uploads/2022/05/next-steps-for-integrating-primary-care-fuller-stocktake-report.pdf (accessed 27 Jun 2023).
Featured photo by Annabelle Machin.