A few weeks have passed since the extraordinary general meeting (EGM) at the Royal College of Physicians (RCP) debating physician associate (PA) roll-out and scope of practice. During the opening presentation, data was shown stating that the majority of PAs are currently employed in primary care settings in England. Dr David Nicholl, one of the RCP fellows responsible for tabling the motions at the meeting, opened his remarks, “We are not primary care physicians” when addressing the college audience. He further alluded to concerns about PAs seeing undifferentiated patients as the first point of contact in primary care. Following the meeting, a number of other controversies were brought to light. The scandal concerning data misrepresentation in relation to surveyed members attitudes to PAs led to the resignation of the RCP registrar.1 Another controversy related to a question from a fellow about the role of PAs in the multidisciplinary team (MDT) seemingly ignored by RCP council members. A third discussed financial and legal implications for the RCP laid out by the treasurer with a tone of implicit pressure for fellows to vote against motion 5 (the motion advocating for a caution in pace of rollout).2 All of the above and many other concerns led to a media storm amongst doctors whilst bringing into focus another talking point – PAs in primary care.
All of the above and many other concerns led to a media storm amongst doctors whilst bringing into focus another talking point – PAs in primary care.
According to data provided by NHS Digital – 1,525 PAs are in integrated care systems (ICS) including secondary care and 1,758 are employed by primary care networks as of 2023.3,4 The obvious question to ask is why NHS England and the RCP feel that it is safer for a group of currently unregulated healthcare professionals with only 2 years of post-graduate training following a “healthcare related” undergraduate degree to be in a position to see undifferentiated patients. It could be argued that at least in secondary care differentiated settings, PAs are far more likely to be integrated into clinical teams and not seeing patients independently. Moreover, the RCP Council’s involvement in decisions relating to PA deployment in primary care without the Royal College of General Practitioners (RCGP) is a mystery in and of itself.
The RCGP have recently made a statement formalising and strengthening their own position on this issue making it clear that PA recruitment should not replace GPs. They stated that shortages of GPs should be addressed alongside supervision requirements for PAs needing wider recognition and resource deployment to be appropriate.5 However, data from Health Education England (HEE) depicts a progressively increasing bottleneck of access to GP specialty training with numbers continuing to rise. In 2016 applications for GPST1 training were 4863 for 3802 posts with a competition ratio of 1.28:1. In 2023 there were 10,514 applications for 3935 posts with a competition ratio of 2.67:1.6
Another compelling factor in this debate involves the introduction of the Additional Roles Reimbursement Scheme (ARRS) in 2019 – a government funded program enabling primary care networks (PCNs) to utilise a funding package to employ additional staff which includes physician associate roles but not doctors.7 Practices cannot use this funding to pay for a qualified GP. The encouragement to hire PAs alongside the lack of funding to hire GPs does not square with political rhetoric that claims to be seeking GPs but not finding them.8
Primary care has been uniquely challenged to limit patient access to an exhausted secondary care system.
A National Institute of Healthcare Research (NIHR) mixed-methods study investigating PA contribution to primary care concluded that PAs deliver similar outcomes to GPs at a lower cost but also made clear that PAs are seeing younger, less complex patients with longer appointment times .9 The study uses patient re-consultation events within 2 weeks as a metric for comparison of effectiveness, despite acknowledgment that patient demographics are completely different – eliminating this as a meaningful comparator. The study also concedes that unrecorded “true supervision” time by GPs means that cost-effectiveness cannot be properly assessed, despite claiming PA consultations are less costly. Furthermore, a systematic review collating available evidence on PAs in primary care notes that most of the studies in this area of research were performed by the same author group with similar research methods allowing for particular data portrayal.10 Declared conflicts of interest in relation to PAs by authors in these papers does not negate the potential for bias in their data collection.
Primary care has been uniquely challenged to limit patient access to an exhausted secondary care system. This is achieved by appropriate triage and excellent safety netting, with a heavy reliance on its clinicians’ clinical competencies. GPs often need to make decisions after a brief consultation without access to ‘objective’ tests to help adjust their personal risk profiling for a patient. For these reasons, it follows that the undifferentiated patient should be seen by those with the most clinical experience – fully trained GPs. Patient care should not be compromised for cost saving or political objectives. The wider public place trust in healthcare professionals to get these things right. Pausing the PA rollout in primary care would help calm the wider social media storm and allow healthcare leaders to make better informed decisions.
References
- RCP publishes pre-EGM member survey data. 18 March 2024. https://www.rcplondon.ac.uk/news/rcp-publishes-pre-egm-member-survey-data [accessed 27/4/24]
- Extraordinary general meeting (EGM) information pack circulated to fellow. 28 February 2024. https://www.rcplondon.ac.uk/news/extraordinary-general-meeting-egm-information-pack-circulated-fellows [accessed 27/4/24]
- Physician associates in primary care by region. 21 December 2023. https://digital.nhs.uk/supplementary-information/2023/physician-associates-in-primary-care-by-region [accessed 27/4/24]
- Physician associates in secondary care by region. 21 December 2023. https://digital.nhs.uk/supplementary-information/2023/physician-associates-in-secondary-care-by-region [accessed 27/4/24]
- RCGP strengthens ‘red lines’ on Physician Associates working in general practice. 8 March 2024. https://www.rcgp.org.uk/News/Red-lines-Physician-Associates-general-practice#:~:text=The%20RCGP’s%20updated%20position%20now,address%20the%20shortage%20of%20GPs. [accessed 27/4/24]
- Competition Ratios for 2023. Medical Hub. Health Education England (HEE) https://medical.hee.nhs.uk/medical-training-recruitment/medical-specialty-training/competition-ratios
- Additional roles: A quick reference summary. 16 May 2023. https://www.england.nhs.uk/long-read/additional-roles-a-quick-reference-summary/
- See https://bjgplife.com/is-there-a-shelf-with-spare-gps-coming-to-the-rescue/ and https://bjgplife.com/amidst-a-gp-workforce-crisis-where-did-all-the-jobs-go/ [accessed 27/4/24]
- Drennan VM, Halter M, Brearley S, et al. Investigating the contribution of physician assistants to primary care in England: a mixed-methods study. Southampton (UK): NIHR Journals Library; 2014 May. (Health Services and Delivery Research, No. 2.16.) Chapter 5, Case studies: evidence from the consultation records and linked patient surveys.Available from: https://www.ncbi.nlm.nih.gov/books/NBK259795/
- Mesharck G. The Role of Physician Associate in Primary Care in England: A Systematic Literature Review. J Med Public Health. 2024;5(1):1097.
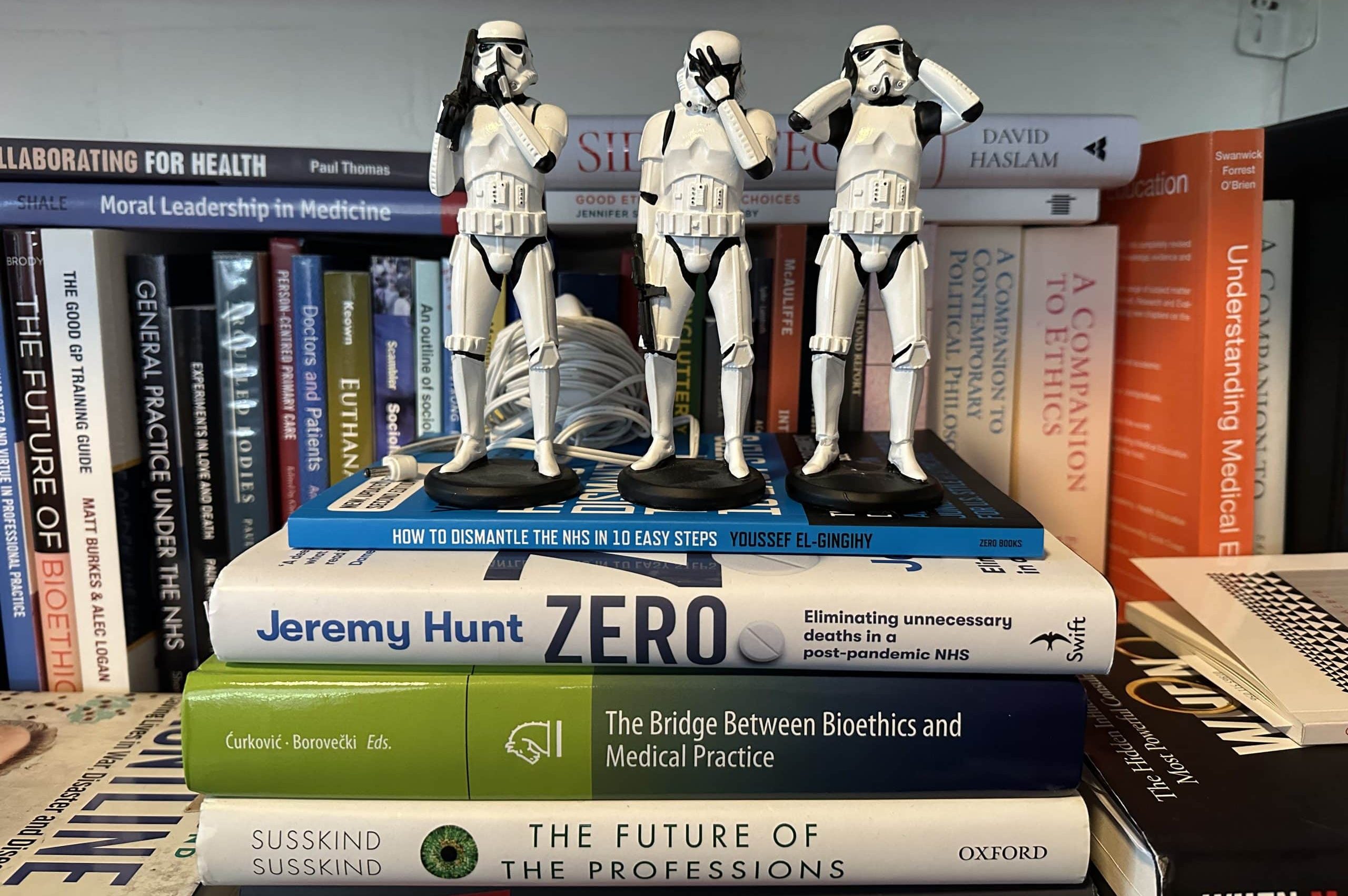
Featured image: The future of general practice? by Andrew Papanikitas, 2023