As BJGP editor I was recently asked (again) to discuss 10 interesting papers from the last year at the Royal Society of Medicine’s general practice and primary care update. These are not, necessarily, the most heavily cited or downloaded, but they do showcase some of the range of topics we cover in the BJGP. Where possible, as it is for an update day, I try to pick papers where there is a key clinical message or it will give some pause for thought on how we deliver care generally.
I can only give a flavour of them here – but click through to the BJGP and read the full articles for any that catch your eye.
At number 10 – heavy menstrual bleeding
Women’s experiences of heavy menstrual bleeding and medical treatment: a qualitative study in primary care,
In some ways, this paper is a good news story – many women were getting, and were valuing, the patient-centred care they got from their GP. Yet, we shouldn’t underestimate how long it takes women to attend and how they may be reticent to disclose details and difficulties with their periods. We have to keep asking.
Heavy menstrual bleeding (HMB) is known to significantly affect women’s health and quality of life, with pressure to conceal symptoms. Recent evidence on women’s experiences of HMB and its treatment after seeking primary care is lacking. This research shows the debilitating impact of HMB on women, and the challenges they can still face, including overcoming taboo and low general awareness that treatment can help. Women had widely differing experiences of current medical treatments for HMB in general practice and emphasised how they valued patient-centred communication in helping them.
At number 9 – hoarding disorder
Hoarding disorder: evidence and best practice in primary care,
Until this was published in the BJGP hoarding disorder (HD) was something of which I knew little – but it was only in 2013 that HD was listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and in 2019 it appeared in the International Classification of Diseases. It’s an interesting disorder and for the GP that gets involved there is likely to be plenty of cross-agency work needed to get people the help they need.
Hoarding is characterised by excessive clutter and difficulty discarding. While many people may report dissatisfaction and difficulties with such symptoms alongside excessive acquisition, only when these lead to clinically significant distress and/or impairment in social, occupational, or other important areas of functioning is the diagnosis of HD considered. Hoarding is associated with significant physical, psychological, and social morbidity leading to reduced quality of life. Even safety can be affected by possessions that congest and clutter active living areas and substantially compromise their intended use. Relationships within the household, with extended family and friends, and even with neighbours may come under strain. HD is found across the world, with a prevalence of approximately 2% and with similar rates for males and females. Despite the prevalence and considerable personal costs, recognising and providing appropriate care can prove challenging.
At number 8 – diagnosing heart failure
Natriuretic peptide testing and heart failure diagnosis in primary care: diagnostic accuracy study,
This papers points that the cut-offs NICE suggest for natriuretic peptide will miss one in five cases – something for the wary clinician to have in mind.
Diagnostic tests are almost always going to be a balancing act between sensitivity and specificity. This papers points that the cut-offs NICE suggest for natriuretic peptide will miss one in five cases – something for the wary clinician to have in mind.
International guidelines recommend natriuretic peptide (NP) testing in primary care to prioritise referral for heart failure (HF) diagnostic assessment. European Society of Cardiology (ESC) and National Institute for Health and Care Excellence (NICE) guidelines differ significantly in their recommended NP referral threshold. The current study found at the lower ESC threshold fewer HF diagnoses were missed but more referrals from primary care would be required. Healthcare systems need to balance the risk of a missed or delayed diagnosis for individual patients with capacity in diagnostic services. An NP level below both the ESC and NICE thresholds was reliable in ruling out HF. Conclusion: At the higher NICE chronic HF guideline NP thresholds, one in five cases are initially missed in primary care but the lower ESC thresholds require more diagnostic assessments. NP is a reliable ‘rule-out’ test at both cut-points. The optimal NP threshold will depend on the priorities and capacity of the healthcare system.
At number 7 – suicide prevention
Suicide prevention targeting middle-aged males: the role of primary care,
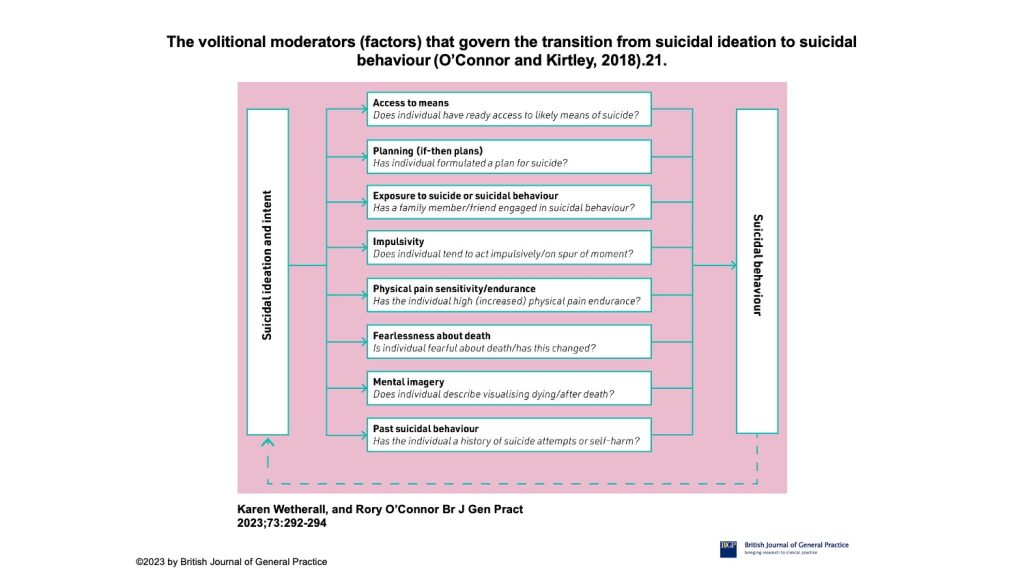
In this editorial, two academics from Glasgow University’s Suicide Behaviour Research Laboratory offer some of the latest thinking on suicide prevention. In particular, the volitional moderators model takes us beyond some of the usual factors and could help us identify those who are more likely to make the transition from intent to action.
Evidence across a range of studies suggests that, on average, 80% of people who die by suicide have been in contact with primary care in the year before dying by suicide, and 44% in the preceding month. Although this represents a significant opportunity for preventative measures, the challenges of identifying who is at risk and how to optimally intervene remain stark. Of all suicide deaths registered in 2021 in England and Wales, three-quarters were by males. Moreover, middle-aged males are the highest risk group, as from 2010 onwards, the suicide rates for males aged 45–64 years are higher than every other age-specific group (20.1 deaths per 100 000 in 2021). Therefore, this group represents an important target for suicide prevention efforts, although age and gender alone are insufficient for suicide risk detection purposes. To address this challenge we need to better characterise risk in this group. The authors discuss elements of suicidal motivations (background factors and triggers), factors that form the intention and enaction of these. They list a set of factors that govern transition form ideation to behaviour including: access to means, planning, impulsivity, exposure to suicidality in others, high pain endurance, fearlessness about death, past suicidal behaviour and mental imagery around death.
At number 6 – withdrawing antidpressants
Withdrawing from SSRI antidepressants: advice for primary care
We have covered this in a number of ways in the BJGP in the past couple of years. We need to recognise that withdrawal symptoms will happen a lot, we need to be able to distinguish them from recurrence of depression and, perhaps the most important message: hyperbolic dose tapering is needed. Some general take home points from the article:
-
Withdrawal is common and can be caused by all classes of antidepressants.
-
Symptoms of withdrawal are diverse, including psychological and physical manifestations. Patients may experience severe symptoms including suicidal ideation.
-
GPs should ask about physical symptoms and consider the symptom timeline to distinguish between withdrawal and relapse.
-
Antidepressants should be tapered through a proportionate reduction regime. This should take place at least over months.
-
GPs should educate patients on withdrawal and the importance of not stopping their antidepressant abruptly.
-
For those who experience withdrawal, GPs should reduce tapering rate, and increase duration while advising on coping strategies.
At number 5 – postural hypotension
Incidence of postural hypotension recorded in UK general practice: an electronic health records study, Cini Bhanu, Irene Petersen, Mine Orlu, Daniel Davis and Kate Walters. 2022; DOI: https://doi.org/10.3399/BJGP.2022.0111
How much postural hypotension is being missed. Quite a lot is the answer according to this study but To the authors’ knowledge, this study provides the first insight into current practice and identification of postural hypotension in routine general practice, assimilating data and trends over a 10-year period.
Standardised recording of postural BP may help increase identification and recording of postural hypotension in GP records. A postural BP drop detected within 60s of standing upright is adequate and more likely to be associated with adverse clinical outcomes. This is a pragmatic approach that could be incorporated into existing routine care for high-risk groups including older adults (such as the NHS ‘Over 75 health check’), and can be carried out by auxiliary healthcare professionals or via ambulatory home BP monitoring, which is now more widely used
Early identification of postural hypotension (that is, before the onset of clinical sequelae such as falls and ischaemic events) may allow for a window of opportunity. This can be used to adjust high-risk drugs, optimise CVD status, and provide practical advice on hydration that may reduce subsequent adverse outcomes.
Finally, postural hypotension and its association with serious adverse outcomes in older people is gaining attention in research. It is recognised as an important marker of neurovascular dysfunction and a contributor to cognitive decline. Therefore, understanding current practice and approaches for improving postural hypotension detection is increasingly important.
Future research should consider age–sex interactions, with greater differences in rates of postural hypotension among males and females in older age groups (>70 years).
At number 4 – hypertension and reverse dipping
Diagnosing hypertension in primary care: a retrospective cohort study to investigate the importance of night-time blood pressure assessment,
This paper highlighted to me the importance of 24-hr BP measurements and the potential limitations of home BP measures. It might be a bit of a pain to organise but there are some good reasons why we might prefer ambulatory blood-pressure monitoring (ABPM) to home blood-pressure monitoring (HBPM).
ABPM has become less frequent in primary care since the COVID-19 pandemic, with HBPM often the preferred alternative; however, HBPM cannot measure night-time blood pressure, and patients whose night-time BP does not dip, or rises (reverse dipping), have poorer cardiovascular outcomes. Researchers used BP data collected for the two cohorts, three systolic BP phenotypes (dipper, non-dipper, and reverse dipper). Not measuring night-time BP puts all groups, other than dippers, at risk of failure to identify hypertension. As a result of this study, it is recommended that GPs should offer ABPM to all patients aged ≥60 years as a minimum when assessing for hypertension.
At number 3 – registering patients without documents
Reluctance of general practice staff to register patients without documentation: a qualitative study in North East London,
It’s not enough to make sure staff know what the rules say about registration – there are moral judgements taking place.
The key point in this study is that staff almost always know what the guidance says about registering people without documents – but they remain reluctant to do so. It’s not enough to make sure staff know what the rules say about registration – there are moral judgements taking place.
Previous research shows that people are often refused GP registration if they do not have access to documentation, highlighting a discrepancy between guidance and practice that has not been previously explored. Current third-sector initiatives to improve inclusive registration have largely focused on reiterating guidance and explaining to staff why people may not have access to documentation. This study found that reluctance to register this group was common, and reluctance was generally fuelled not by lack of knowledge of the guidance, but by workplace and resourcing pressures, and moral judgements concerning who should be entitled to NHS services based on immigration status. The perceived practical and financial burdens relate to overall increases in workload and the current funding model utilised in general practice. Initiatives to improve access must acknowledge such concerns, alongside addressing the wider malignant impact of the ‘Hostile Environment’ policies on individual staff decision making.
At number 2 – treatment burden and ‘missingness’
Treatment burden for people experiencing homelessness with a recent non-fatal overdose: a questionnaire study,
Editor’s Choice: At number 1 – wax on, wax off
Ear wax management in primary care: what the busy GP needs to know,
There are a few reasons I plumped for this Clinical Practice article. After some comments about access to general practice which gave the opportunity to be a little self-righteous and pompous, it felt important to lighten the tone a little. Yet, this is a serious topic and one that can cause a lot of distress for patients. It is also one of our most downloaded papers of the year so it’s clearly attracting some interest.
Perhaps one of the key messages is that there is a lack of good evidence to guide care but from what can be gleaned here are some take home messages:
-
A significant number of people fail to get the care they need for earwax removal and there is an urgent need for such a service in primary care.
-
Pre-treatment softeners are recommended followed by removal using electronic water irrigation or microsuction.
-
The use of modern portable equipment within a primary care network and for use in care homes is a possible approach.
-
Groups of practices rather than each individual practice can collaborate as primary care networks to provide a range of services, such as earwax removal. The cost of setting up a video-assisted mobile earwax suction service within a group of practices would involve an initial set-up and training cost-of around £1000, and any ongoing cost associated with rental of mobile equipment. However, the feasibility, clinical and cost effectiveness of this care pathway needs testing in an RCT.
Featured photo, BJGPs on a table, by Andrew Papanikitas, 2023. The text in italics are quotes from the articles.