Afsana Bhuiya (pictured) is cancer GP lead for the NCL Cancer Alliance, GP in Barnet (HWS), NCL Clinical lead (Fertility policy and EBI), and GP Appraiser. She is on twitter: @afibhu
Afsana Bhuiya (pictured) is cancer GP lead for the NCL Cancer Alliance, GP in Barnet (HWS), NCL Clinical lead (Fertility policy and EBI), and GP Appraiser. She is on twitter: @afibhu
Dr Sarah Dougan is Director of population health intelligence, North Central London CCG
Omid Hajimirsadeghi is Senior Content Solution Designer, Cerner Harriet North, Lead Principal Population Health Analyst, Camden and Islington Public Health
“What is population health?”
“What is population health management (PHM) and what is a PHM registry?”
“Why are these things useful and to whom?”
Those of us who work across various parts of the health system have reflected how many ‘population health’ terms are received with confusion amongst some clinicians and managers. Below, we address some of this confusion by clarifying answers to these questions and showcase the clinical context by examples.
Population health, is at its core, about improving and promoting health across an entire population, and the management aspects describe how health and care workers can together understand and effect the appropriate care for the population they are charged with. Improving the health of the entire population is not an easy undertaking. It takes significant political and cultural change to embed the PHM approach. Understanding the population you are charged with is fundamental to knowing what to improve and supporting this task are digital PHM tools. These enable data to be aggregated, consolidated and analysed to create a comprehensive clinical picture of the population and of the patient.
In North Central London (NCL), as in many other areas across England, we have a digital provider (Cerner) who provides the overarching integrated digital care record and analytic tools such as dashboards and registries.
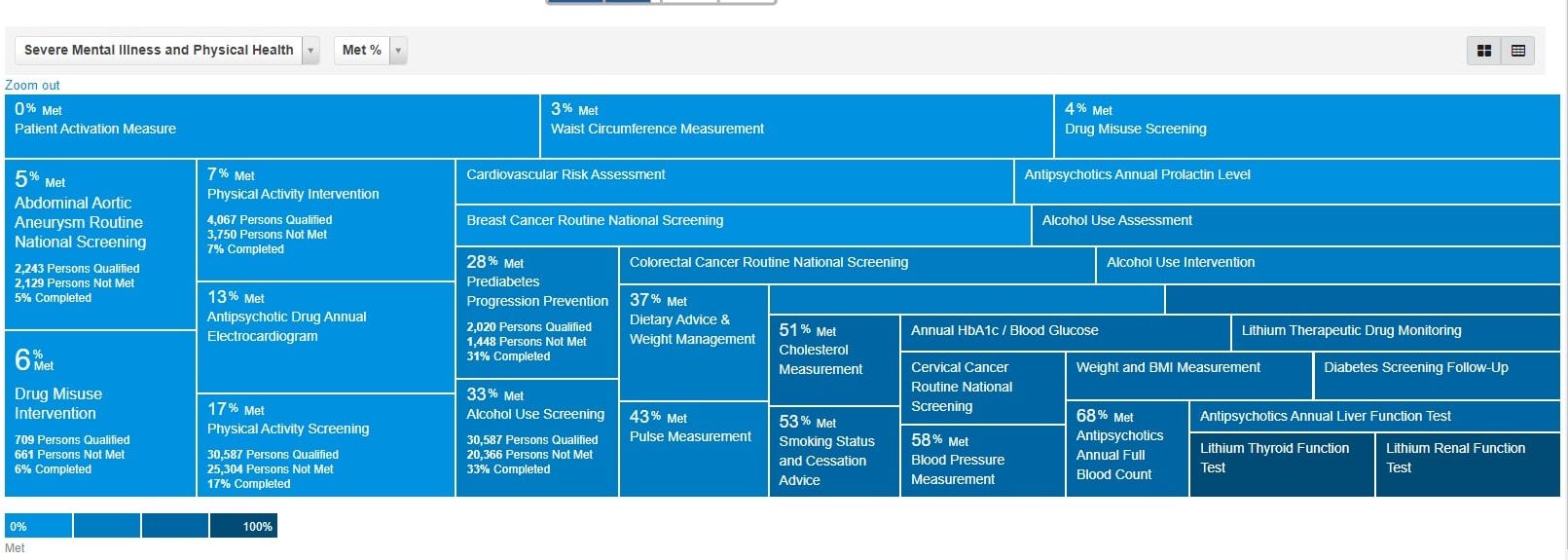
…dashboards… present data visually so that users can understand it better, patterns can be detected that otherwise may not have been noticed.
They present data visually so that users can understand it better, patterns can be detected that otherwise may not have been noticed. A recent example of high-impact use is where COVID-19 vaccination dashboards support the vaccination programme. Dashboards are are already embedded into quality improvement work across the healthcare setting. Importantly, tools like this can help spotlight inequalities in provisions and uptake so targeted approaches can be taken.
PHM registries build on the dashboard, offering an extension to data collection and analysis based on a group with shared characteristics. Registries, or the various other synonymous terms for it, like – quality registries, clinical databases – essentially collect standardised information on patient diagnoses, care processes and outcomes. The registries enable systematic comparison and analysis and are often presented in a dashboard view to show how patients measure up against different agreed quality standards. The quality of the data is an important part of the picture and integrating health and care records across primary and secondary care to create the registries is a powerful advancement, We are using collective data at scale and the aspiration is to understand our patients, improve their care where needed, reduce inequalities for those we see falling between the cracks and proactively plan care and services in an ongoing iterative way using quality improvement approaches.
PHM registries are established for some long term conditions, where there are well defined quality markers and indicators of care, such as Diabetes or COPD. Then there are more novel registries supporting serious mental health conditions and cancer care./
Our reflections relate to creating a PHM cancer care registry for the NCL population. The registry work started in 2019, its focus is on the adult population in the NCL geography who have a cancer diagnosis.
Registries offer a data-informed baseline understanding of a specific group of people.
The cancer care registry use case has arisen from the fact that more people are getting cancer and living longer with more complex needs. A well-floated statistic states one in two people will get cancer sometime in their life and with a predicted rise of people living with cancer in the UK from two point five million to four million by 2030, the number of people having experienced cancer or living with cancer cannot be ignored. Cancer treatments are expensive and can have long-term effects on people years after treatment. A further complexity that cancer patients can face is that up to seventy percent of this group have at least one long term condition. For those working on cancer, the strategic aspiration is to have cancer established as a long term condition. The recent NHS long term plan cements the personalised care model for patients with cancer, who need such a personalised approach.
In early 2022, the cancer care registry will launch and this could be a key enabler to support higher quality care for this group. The registry will capture key cancer care specific metrics such as cancer care reviews, cancer care planning and treatment summaries to wider health and social data around frailty, mental health screening and next of kin. The registry will allow service providers in primary care to analyse these patients as a collective, against these care standards. We know primary care maybe well placed to deliver a PHM approach in view of the general holistic nature of the work.
Registries offer a data-informed baseline understanding of a specific group of people. Once we can understand their needs and gaps in care provision and see these across various characteristics (protected or otherwise), we can address these and do it is a tailored way.
We are really looking forward to explore the potential of this new tool and aim to bring back our key findings and learnings to the wider audience.
Featured image: Screen-shot of severe mental illness and physical health registry by Afsana Bhuiya