
Watch his video: Dealing with COVID-19 in US family medicine
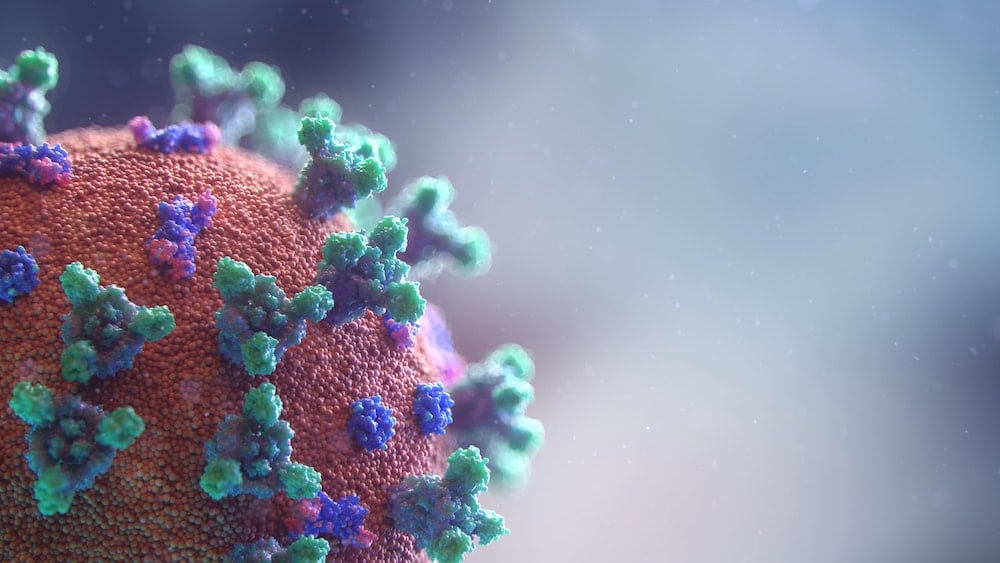
Coronavirus is exposing and exaggerating deep inequities in our society. The COVID-19 hot spots of disease burden and mortality also reflect different types of hot spots. Even though it is clear that viruses do not discriminate, data from across the US and UK demonstrate that the neighbourhoods of colour are impacted differently by COVID-19. Almost daily the news and medical journals report the disparities in test positivity, hospital admissions, ICU cases, and death. But why?
Something very unusual is happening on both sides of the Atlantic where the US has the world’s highest number of fatalities and the UK has now topped 30,000 deaths, the most in Europe. A recent UK report° found black women and men are over four times more likely to die with COVID-19 than whites. The most recent US CDC report° revealed that over 30 percent of COVID-19 patients are African American yet make up about 13 percent of the population.
Counties with higher black populations account for more than half of all COVID-19 cases.
Why are so many dying? Certainly Louisiana is a hot spot in obesity with a nearly 40% percent obesity rate, as well as a hot spot for the co-morbidities of diabetes, cardiovascular disease, hypertension, and kidney disease. The same is true for the hardest hit neighbourhoods in the other cities. Many of the victims suffer more than one of these conditions. Vitamin D deficiency is also being connected to poor outcomes° and tied closely to darker skin groups.
Beyond the medical model — the structural social hot spots
Dr. Jerome Adams, US Surgeon General stated on CBS in April: “Blacks are more likely to have diabetes, heart disease, lung disease… and many black Americans are at higher risk for Covid-19.” On a later CNN podcast Adams then states: “My recommendation is to all of America that we’re really doing this [staying home/distancing] to protect not just ourselves but each other. Every single person who stays at home is a person who is not spreading COVID-19… ”
But can the simply stay home rule and safe distancing apply equally to the communities of colour where structural inequities exist? The virus hits communities differently and the hot spots of poor health and socioeconomic disparity are mirroring the COVID-19 hot spots.
Living spaces are overcrowded making distancing all but impossible. Working and schooling from home is often not an option. “Essential jobs” in the service sector are overrepresented by minorities creating more chances for exposure — jobs such as home health aides, grocery work, delivery, and services. Economic hardship exacerbates stress as the pandemic is having devastating effects on jobs, future earnings, the immediate threat of lay off, and future health insurance coverage. There is a wage gap for minorities and often little to no savings to support financial gaps from distancing. It’s hard to get away from being poor.
Many minority neighborhoods are food deserts with little to no access to affordable nutrient dense foods.
Cases might be under reported as there is often limited access and resistance to enter health care. Thus far testing been a clinical strategy of case identification of symptomatic people versus a public health approach. We need racial and ethnic data to help us identify current and future communities at risk. Greater disease rates are rooted in socioeconomic, physical and even psychological factors such as chronic stress.
It’s not all negative. Bright spots in education are happening with improved home computer and internet access. States are enacting task forces to address disparities. We can build back stronger communities. Hurricanes Katrina and Sandy have hopefully taught us lessons. Knowledge leads to public policy change and public health preparedness to address the disparity hot spots as we learn to live with COVID-19.






[…] is at historic highs -Coronavirus is affecting communities of color at much greater rates. I wrote a piece on this crisis here -as the country starts to gradually reopen fears of financial insecurity and economic crisis are […]
[…] https://bjgplife.com/2020/05/20/the-differential-impact-of-covid-19-on-neighbourhoods-of-colour/ […]