Both dementia and COVID-19 have been identified as urgent public health priorities by the World Health Organization.1,2 In England, the first COVID-19 national lockdown began on 23 March 2020, while recent political commitments have pledged to improve early diagnosis in people living with dementia.3
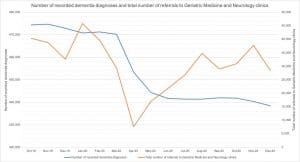
NHS England publishes monthly data on the national number of recorded dementia diagnoses.4 From March 2020 (470,292) to May 2020 (444,442) there was a 5.50% decrease in the number of diagnoses. There was a similar 5.48% decrease when comparing May 2019 (470,234) with May 2020. The number of diagnoses has since remained stable from June 2020 (441,752) to December 2020 (438,361) (most recent available data).
Public Health England publishes weekly data on mortality in England.5 In total, 25,244 patients died in April 2020 and May 2020 with ‘Dementia and Alzheimer’s disease’ recorded on their death certificates. This was more than double the expected number compared with the 5-year mean for April and May, and is similar to the absolute decrease in the national number of dementia diagnoses during these months (25,850).
These data suggest that the backlog of patients with suspected dementia.
NHS England also publishes monthly data on the number of referrals to specialist services from primary care.6 GPs can request specialist assessments for patients with suspected dementia by referring to Geriatric Medicine or Neurology clinics (the proportion of these referrals that specifically request dementia assessments is unknown). Compared with March 2020 (29,369), the total number of referrals to these specialist clinics decreased by 74.01% in April 2020 (7,634), and by 42.27% in May 2020 (16,956) (no data prior to October 2019 available for comparison). Monthly referrals returned to baseline in August 2020 (34,728) and have remained stable since.
In summary, both the number of patients living with dementia, and referrals for specialist dementia assessments, substantially decreased in April 2020 and May 2020, coinciding with the first COVID-19 lockdown. The number of recorded dementia diagnoses has since remained stable, and monthly referrals for dementia assessments returned to pre-lockdown levels in August 2020. Crucially, the rate of referral has not exceeded beyond this baseline (see table).
These data suggest that the backlog of patients with suspected dementia, caused by pandemic-induced health service interruptions, has not yet been referred for specialist assessment. An above-baseline rate of referral would reflect the processing of this outstanding disease burden, but has so-far not materialised. This implies a substantial increase in the number of patients living with undiagnosed dementia, and is reflected in the estimated dementia diagnosis rate (the proportion of those aged 65 or over estimated to have dementia who have a coded diagnosis of dementia in their primary care record) decreasing from 67.4% (95% CI 60.7-73.0) in March 2020 to 62.4% (95% CI 56.3-67.6) in December 2020.4
The impact of living with dementia on physical, mental and social health is profound, while formal diagnosis provides a suite of potential benefits for both patients and families.7 There is therefore urgent need for primary care practitioners to identify and refer those suspected of living with dementia. Strong public health messaging, proactive case-finding, and community awareness campaigns are required to reverse the impact of COVID-19, re-establish early diagnosis as a national priority, and rekindle global efforts to combat dementia as a significant threat to public health.
References
- World Health Organization and Alzheimer’s Disease International. Dementia: a public health priority. 2012. https://www.who.int/mental_health/publications/dementia_report_2012/en/ [accessed 21 January 2021]
- World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 30 January 2020. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [accessed 21 January 2021]
- Department of Health and Social Care. Prime Minister’s challenge on dementia 2020. 21 February 2015. https://www.gov.uk/government/publications/prime-ministers-challenge-on-dementia-2020/prime-ministers-challenge-on-dementia-2020 [accessed 21 January 2021]
- NHS Digital. Recorded Dementia Diagnoses. https://digital.nhs.uk/data-and-information/publications/statistical/recorded-dementia-diagnoses [accessed 21 January 20212020]
- Public Health England. Excess Mortality in England. https://fingertips.phe.org.uk/static-reports/mortality-surveillance/excess-mortality-in-england-latest.html [accessed 21 January 2021]
- NHS England. NHS e-Referral Service Open Data October 2019 to October 2020. https://digital.nhs.uk/data-and-information/publications/statistical/mi-nhs-e-referral-service-open-data/oct-2019-to-october-2020/data-tables [accessed 21 January 2021]
- G Livingston, J Huntley, A Sommerlad, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet 08 August 2020; 396(10248): 413-446. DOI: https://doi.org/10.1016/S0140-6736(20)30367-6
Featued photo by Robina Weermeijer at Unsplash