 Stephen Gillam is a semi-retired GP and public health specialist who has written extensively in both fields. He is the author of ‘Of Patient Bearing – A History of General Practice in Eight Generations.’
Stephen Gillam is a semi-retired GP and public health specialist who has written extensively in both fields. He is the author of ‘Of Patient Bearing – A History of General Practice in Eight Generations.’
Introduction
Major developments in the public funding of health care were to take place over the next two generations of my family. The Liberal Government of Herbert Asquith initiated the birth of our modern welfare state through educational reforms, the introduction of old age pensions and, crucially, national health insurance. These reforms had multiple causes including heightened awareness of the causes and consequences of poverty. These had been graphically demonstrated by the poor physical state of working class recruits for the Second Boer War. The creation of health insurance followed German precedents and its influence on general practice was profound.
The National Health Insurance Act of 1911 established a system of free health care financed by tripartite payment from those in employment, from employers and the state. Thenceforth, general practice covered workers but not their wives and families, whose demands were curtailed by the need to pay fees for service.1 Access to GP care steadily widened but that care was of variable quality. These reforms nevertheless impacted positively on the financial viability of my great grandfather Joseph Gillam’s (1870-1911) practice.
The early 20th century ‘consultation’
Diagnosis was imprecise with little use of examination or instruments and a tendency to over-prescribe.
GPs in poor, inner city communities recalled the waiting room containing rows of seats for dozens of patients who sat facing a high bench like a bank counter. Behind this counter stood the doctor and behind him the dispenser. The doctor called the next patient to come forward. Having listened to the complaint, he turned to the dispenser and ordered the appropriate remedy. These ritualised encounters of three to five minutes emptied waiting rooms but left little time for preventive advice. Cheerfulness, a hopeful demeanour and sympathy were all important. ‘Laying on of hands was the important thing…medicine was 70 per cent art and 30 per cent science’.2 There was rarely any attempt at examination. Daily visits often numbered over fifty and were mostly made on a bicycle.
Clinical practice was slow to change and traditional practices endured. Diagnosis was imprecise with little use of examination or instruments and a tendency to over-prescribe. The dissemination of best practice was variable and constrained by the economic and social context of individual practices. Middle class fee-paying patients got more extensive investigations and better medicine. Doctors’ expanding knowledge of symptoms and signs aided the diagnosis of common diseases. Other positive advances included minor surgery and the first effective drugs.
Successful treatment by the family doctor was accepted with gratitude and their many failures were tolerated with little rancour or recrimination. Patients’ expectations were not high. Pain and discomfort were accepted as part of life to be endured with stoicism.3 The death of children from infectious disease was the way of the world. Mothers of feverish children expected, if the child was not to be admitted to the fever hospital, to be told that bed rest was crucial until the fever had fully subsided. GPs’ hours were long, as most practices were single-handed and deputising services were non-existent.
The new ‘Lloyd George’ record cards introduced with NHI effected a revolution in medical note-keeping. Analysis of early cards suggests that clinical notes were made only for the minority of more serious conditions requiring sickness certification, referrals or surgery. Diagnoses were overwhelmingly in physical terms and few clinical measurements or investigations were recorded. These records therefore provide only partial insights into the true frequency of conditions encountered.
Medical diagnosis was anyway often of academic rather than practical importance. Treatments were still limited to thyroid extract, iron, digitalis, barbiturates, simple analgesics, morphine derivatives and harmless mixtures. Insulin, liver extract for pernicious anaemia and new mercurial diuretics only became available in the 1920s.
The advent in the mid-30s of sulphonamides and then penicillin were transformative. Sadly, this was too late for my grand-father Joseph who, after eight days visiting his patient in expectation of ‘the crisis’, succumbed to the same pneumonia aged 42. Woods’ study of medical mortality from 1860-1911 shows that general practice was a particularly dangerous trade.4 The risk of contracting infections such as TB from your patients was ever-present. The dangers of home visiting on horseback, of addiction to drugs and alcohol, of vulnerability to depression and suicide from readily available drugs, all contributed to high death rates. Many doctors could not afford to retire and simply died ‘in harness’.
Domestic ideology
The invisibility of women in accounts of the time, other than as mothers, is shocking to contemporary sensibilities.
The invisibility of women in accounts of the time, other than as mothers, is shocking to contemporary sensibilities. However, the separation of work and home was less and less absolute. Women were a ‘hidden investment’ whose labour was essential to the success of many small businesses.5 General practices were no exception. Wives were crucial to the practice’s success combining the duties of receptionist, telephonist and secretary. A spouse chosen from an elite family might strengthen the family socially or financially. Wives could bring capital to businesses – as later did my grandmother and great-grandmother. Sentimental images of nineteenth century family life belie how strategically complex was the maintenance of class and professional privilege.
The creation of the NHS
There is a tendency to assume that the National Health Service Act was the culmination of a single clear idea, realized in a glorious post-war dawn; the reality was messier. There was growing consensus in the years leading up to the Second World War that existing services were inadequate and unsustainable. The outbreak of war necessitated the creation of an Emergency Medical Service (EMS) for the wounded. The EMS is credited with establishing an embryonic health service and facilitating nationalization.6 The War itself reinforced support for expansion of the state’s social and economic responsibilities.
By 1941, some 21 million people were provided care under the National Insurance Act and two-thirds of GPs were participating in the panel system. William Beveridge (1879-1963) laid the foundations for the new service in his eponymous report the following year. He provided a blueprint for post-war welfare reform while the landslide Labour victory of 1946 allowed for its realization. The NHS Act 1946 finally provided a family doctor to the entire population. The new service was tax-funded, accessible to all and free at the point of delivery. Nationalization of existing voluntary and municipal hospitals was effected and Lloyd George’s insurance scheme extended to all.
Rose-tinted historiography in support of Beveridge’s vision have tended to obscure shortcomings in the new National Health Service which swiftly ran into difficulties at a time of austerity.
The establishment of the NHS involved inevitable compromises leaving certain tensions unresolved, e.g. between local government control and national government’s responsibility, between public accountability and professional participation. Notably, the price for Bevan of hospital consultants’ accepting salaried contracts was continued private practice while GPs remained outside the service altogether as independent contractors. GPs, fearing that they might be no more than officials in a state service, had argued successfully for a contract for services rather than a contract of service. As a result, they remained self-employed, organising their own professional lives.
Early years, early challenges
Rose-tinted historiography in support of Beveridge’s vision have tended to obscure shortcomings in the new National Health Service which swiftly ran into difficulties at a time of austerity. Costs were expected to peak in the face of new demands, then fall as these were met. Unsurprisingly, both demands and costs continued to rise. There was a desperate need for investment in plant. The quality of care was variable, particularly in inner cities.
For general practitioners, the NHS represented an elaboration of the system of National Health Insurance under which a capitation system also operated. Many detailed NHI regulations were simply transferred into the NHS. There were limited economic incentives to provide good patient care; lists were kept long and costs low. The standards and social ethos of care were largely a continuation of the old panel system. Workloads rose with the incorporation of more women and children onto patient lists and the expanded take-up of free health services. The tide of health reforms left GP morale at a low ebb. Some considered the future of general practice itself to be in jeopardy.7
The infamous Collings report exposed wide and unacceptable variation in standards.8 Collings laid out a detailed and costed plan both at practice and at national level. He discussed the staffing, the architectural design of premises, the financial inducements required and the financial advantage to government: the better general practice became, the less the burden on expensive hospitals.
GPs’ situation nevertheless combined private enterprise and state service without the characteristic advantages of either. They could not reap the rewards of building up a practice, and the better they did the work the worse off they were. Money spent on premises, equipment and staff diminished their income. Mr Justice Danckwerts was commissioned to examine GPs’ pay and his report of March 1952 proved to be a portent of change.9 Within three months there was agreement on raising the flat capitation rate to increase recruitment, an initial practice allowance to make it easier for new doctors to enter practice, and financial encouragement to form partnerships and group practices.
A Royal College at last
In November 1952 the College of General Practitioners was finally formed. As usual, it encountered strong opposition from the Royal Colleges of Physicians, of Surgeons and of Obstetricians and Gynaecologists. The College aimed to encourage high standards of service, teaching and research. Central to the College vision was that family medicine had its own skills and knowledge base that were as important as anything the hospital services might bestow upon it. The work of men such as Michael Balint, a psychoanalyst, was central to this. Balint, at case conferences at the Tavistock, cast new light on the nature of the consultation and was an important figure in the establishment of general practice as a discipline in its own right. He argued for a different type of education and research, regarding the relationship of the GP and the consultant as a perpetuation of the pupil-teacher relationship.10
One of the College’s first initiatives was to see what medical students were taught about general practice. Although medical students from a number of schools visited practices, only Manchester and Edinburgh had teaching units in the medical school. It was the beginning of a struggle to attain recognition of general practice as a subject entitled to a place in the overcrowded student curriculum.
The College was granted its Royal Charter in 1972. Its lasting impact on education and training standards has been enormous. Nowadays membership via examination is an absolute prerequisite for entering the profession. The College journal exemplifies the extent to which the academic foundations of general practice have been transformed. Latterly, the College has also raised its political profile as an effective advocate for the discipline.
Conclusion
GPs’ fortunes continued to fluctuate and varied geographically. It was particularly hard to sustain both performance and income in poorer areas.
If the doctor moved from the margins to the mainstream of social life from 1850 to 1900,11 the medical profession underwent its most meteoric development between 1900 and 1950. NHI was a necessary interim stage in the evolution of the right of citizens to health care – in many respects, more revolutionary than the formation of the NHS.
NHI provided some financial security for doctors like my great uncle Henry Skrimshire (1874-1953) who took over the practice in Holt when Joseph died. He cared for workers but not their wives and families, whose demands were curtailed by the need to pay. Like many others, Harry operated his own welfare system waiving fees for the indigent.
The advent of the new national service afforded generalists such as my grandfather Geoffrey Gillam (1905-1970) unforeseen opportunities to develop their careers. He moved from general practice in Bungay to become a cardiologist.
Overall, the early years of the NHS had seen remuneration stagnate and morale (ever a commodity that general practitioners could talk down) decline. Jobbing GPs felt that they were held in little respect. GPs’ fortunes continued to fluctuate and varied geographically. It was particularly hard to sustain both performance and income in poorer areas. On the other hand, these reforms had brought fewer changes than GPs might have feared. Therapeutic advances were all the while extending the range of conditions that family doctors could manage effectively. The stage was set for another upturn.
This article is one in a five-part series: A short history of general practice:
- Professional roots https://bjgplife.com/a-short-history-of-general-practice-professional-roots/
- The coming of family practice https://bjgplife.com/a-short-history-of-general-practice-the-coming-of-family-practice/
- Servants of the state https://bjgplife.com/a-short-history-of-general-practice-servants-of-the-state/
- Consumerist medicine https://bjgplife.com/a-short-history-of-general-practice-consumerist-medicine/
- The changing gaze https://bjgplife.com/a-short-history-of-general-practice-the-changing-gaze/
References
- Gilbert B. The Evolution of National Insurance in Great Britain: The Origins of the Welfare State. London: Michael Joseph, 1966.
- CMAC, GP 24/2/48, Bertie Dover. Quoted in Digby A. The Evolution of British General Practice, 1850-1948. Oxford: Oxford University Press, 1999.
- Pooler H. My Life in General Practice. London: Christopher Johnson Publishers, 1948.
- Woods R. Physician Heal Thyself; the Health and Mortality of Victorian Doctors. SHM 1996; 9: 24-30.
- Davidoff L, Hall C. Family Fortunes: Men and Women of the English Middle Class, 1780-1850. London: Routledge, 2002.
- Klein R. The New Politics of the NHS. 6th Oxford: Radcliffe Publishing, 2016.
- Anthony E. The GP at the crossroads. BMJ 1950; 1: 1077-9.
- Collings JS. General practice in England today. A reconnaissance. Lancet 1950; 1: 555-79 + appendices.
- Webster C. The Health Services since the War, I Problems of Health Care: The National Health Service before 1957. London: HMSO, 1988.
- Balint M. Training general practitioners in psychotherapy. BMJ 1954; 1: 115-20.
- Harris J. Private Lives, Public Spirit. A Social History of Britain, 1870-1914. Oxford: Oxford University Press, 1993.
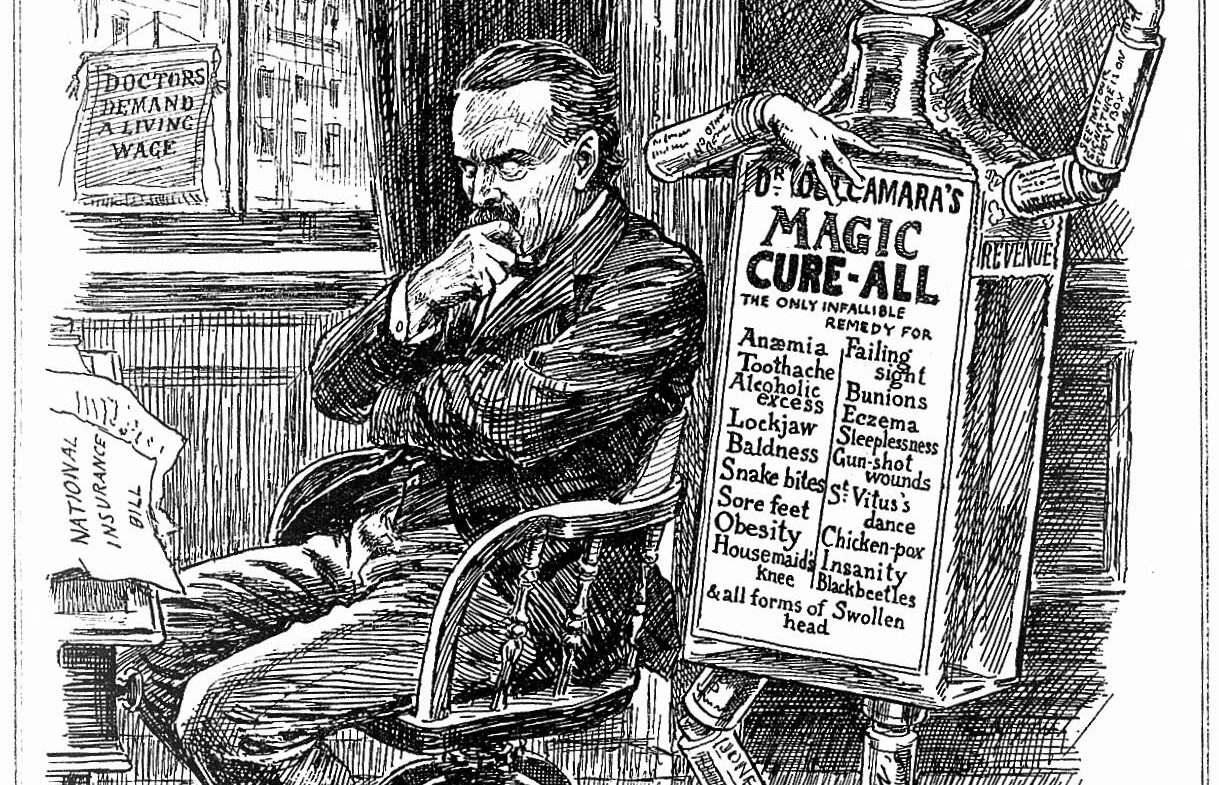
Featured image: A figure comprised of medicine bottles and tablets, representing the patent medicine business, dances behind a pensive Lloyd George; representing attitudes to the introduction of the National Insurance Act of 1911. Wood engraving by B. Partridge, 1912.. Credit: Wellcome Collection. In copyright








Stephen Gillam is a semi-retired GP and public health specialist who has written extensively in both fields. He is the author of ‘Of Patient Bearing – A History of General Practice in Eight Generations‘ and winner of the RCGP and Society of Apothecaries Rose Prize in the history of British general practice.
Introduction
Over time, new scientific discourses have shaped the way doctors view their patients.1,2 Movements in epidemiology, social and behavioural sciences, management theory, political and moral philosophy change doctors’ perception of ‘what is wrong’ and ‘how we know it’.3 These disciplines have left their own distinct sedimentary stains of language, values and practice. What my forebears ‘saw’ changed down the generations.
The apothecary William Skrimshire (1739-1814) received no formal training. He practised in the marshy hamlets and villages around Wisbech where malaria and other marsh fevers were a scourge. He studied texts still imbued with miasmatic theory and humoralism. The emphasis on prevention and behavioural change was stronger then and many of his recommendations regarding the ‘non-naturals’ would resonate today. His son, also William (1766-1829), was the first to attend medical school, in Edinburgh. Natural sciences were central to medical education and he developed a lifelong passion for botany, bequeathing an extensive herbarium on his death.
Over the next generations, medical discourse became recognizably biomedical. As doctors are still wont to do, my great great grandfather John Truscott Skrimshire (1835-1912) and his sons discussed their ‘cases’. As a boy, I watched my father and grandfather, with clinking whiskies to hand, standing either side of the sitting room fire doing the same. Nowadays, it is regarded as a lapse of taste to refer to patients as ‘cases’, as though they were the receptacle inside which the doctor’s true object (the name of the disease) is concealed.
The second article in this series described the emergence of the ‘family doctor’, a stereotype which proved enormously powerful in shaping public and professional perceptions of contemporary practice.4 This coincided with rise of laboratory medicine during the second half of the nineteenth century. The term ‘laboratory’ refers not just to physical space but to associated attitudes and methodologies. In the advancement of basic medical sciences, German universities led the scientific research community. The advent of medical microscopy gave rise to competing epistemologies of disease. Traditional diagnosis based on histories and observation was displaced by a new ‘rational medicine’ based on histology. Medical authority shifted to the pathologist as the final diagnostic arbiter and the laboratory came to be regarded as the source of most fundamental, reliable information on the workings of the body.
Major developments in the public funding of health care were to take place over the next two generations. The National Health Insurance (NHI) Act of 1911 established a system of free health care financed from employers and the state. My great uncle Henry Skrimshire (1874-1953) cared for workers but not their wives and families, whose demands were curtailed by the need to pay. NHI provided doctors with some financial security and, like many others, Harry operated his own welfare system waiving fees for the indigent. My grandfather Geoffrey Gillam (1905-1970) worked either side of the establishment of the NHS; general practice was reorganised but not transformed.
Till half a century ago, the psychological was regarded as the antithesis of the physical – a distraction that seduced the doctor from fidelity to the clinical task. ‘I make it an absolute rule never, under any circumstances, to tell a patient what his blood pressure is. Instead I say ‘not bad for your age’, or ‘quite reasonably satisfactory’. Once a patient knows he or she has hypertension, symptoms multiply enormously, and misery grows…’5 Practitioners such as Stephen Taylor disdained psychologizing; the diagnostic prizes were the diseases he first encountered at medical school.
Psychodynamic approaches to consulting gathered momentum in the 1960s onwards, in tune with the individualistic spirit of the period.6 Michael Balint readjusted practitioners’ clinical focus: first from disease diagnosis to the meaning of the illness, secondly from the illness to the patient, thirdly from the patient to the doctor-patient relationship.7Biopsychosocial approaches to teaching moved centre-stage in 1970s.8 They framed diagnosis in physical, psychological and social terms. This represented a major break from the established instrumental, hospital-centred orientation but general practitioners’ preferred default remained biomedical for that is the basis on which they are schooled, selected and trained.
‘A profound problem is that the map of biomedical science only roughly matches the territory of human suffering.’ 9 My uncle Pat (for whom I undertook locums) was a single-handed general practitioner working round the clock on the Pembrokeshire coast. He resembled no-one so much as John Sassall, the subject of John Berger’s acclaimed meditation on humanity, society and the value of healing.10 A Fortunate Man is a memorial to a way of practising medicine – for many a high watermark – that is nowadays impossible to sustain.
The 1980s saw a steady resurgence of the preventive agenda.11 ‘Illness became a prediction, a variable probability, a genetic weakness or a human frailty in behaviour, in which treatment must be invested now, in the expectation of benefit later.’3 Julian Tudor Hart, most notably, sought the fusion of epidemiology with primary care.12 Illness was once more re-located from ‘in here’ (the body-mind) to ‘out there’ in the socio-economic characteristics of the community.
General practitioners’ public health role was further extended from the 1990s onwards. My generation engaged in commissioning on behalf of practice populations. This inevitably shifted our ethical compass away from one-person clinical medicine. Ironically, there were intriguing similarities in the language of Tudor Hart and proponents of the health care markets he so abhorred. The authors of Working for Patients talked of producers and consumers.13 For Tudor Hart, the consultation was the point of ‘co-production’ of important health-related consumptions.12
The evangelists of Evidence Based Medicine were unwitting foot soldiers in this brave new world. Quantification as an aid to decision-making fostered a growth industry in the production of guidelines, protocols and algorithms. Criteria for diagnosis, investigation and treatment were henceforth determined by combing the world literature for evidence. The randomised controlled trial came to exercise a tyrannical domination over other intelligence. Economists refined a calculus of cost and benefit in the search for a morally neutral basis for rationing decisions. This reached its apogee in the Quality and Outcomes Framework with its unitary measure of quality.
Whither now the ‘family doctor’? We remain attached to the idea for the connotations of intimacy and extended biography it suggests. It is hard to ignore the influence of family on presentation, diagnosis and management. Huygen14demonstrated how new generations learn how to be ill from their parents. However, critics have drawn attention to the inherent conflicts of interest and confidentiality between different members of the family and household.15
Other changes have continued to erode family practice: the end of round the clock responsibility; the growth of part-time salaried practice; declining rates of home visiting, the source of so much intimate knowledge. The associated administrative demands of pay-for-performance, commissioning and regulation have crowded out the style of practice upon which the popularity of the discipline was founded. Less personal care is the consequence. My working life has seen a steady decline in the status of generalists, despite impressive therapeutic advances.
A new cosmology
Over forty years ago, Nicholas Jewson coined the term ‘medical cosmology’ as shorthand for the prevailing theories and practices that defined the nature of medical discourse at that time. He argued that, until the late eighteenth century, a system of ‘bedside medicine’ had prevailed in the western world. An individual’s psychological and social circumstances, behaviours and life history were central to diagnosis and treatment. A new cosmology emerged from post-Revolutionary France in the form of ‘hospital medicine’. It employed concepts and technical language that were increasingly alien to lay understandings. This, in turn, was supplanted by ‘laboratory medicine’ which sought disease at the cellular level and intensified the reductionist tendencies of the preceding stage.16
Arguably, we are now grappling with a new cosmology, that of ‘virtual medicine’, which will once more shift what Jewson called the ‘locus of epistemological authority’. The medical gaze is nowadays refracted through computerised protocols and algorithms; first we check the template, then we listen to the patient. The screen has replaced the body as the emblem of contemporary medicine. Actual practice is no longer tactile. We scan before we undertake physical examinations. If we lay on hands at all, we do so for largely symbolic reasons. The subjective sense of illness and bodily unease arising from disease, tiredness and unhappiness has been invalidated by scientific medicine with its emphasis on disease.
Personalized medicine is taking a paradoxical turn, redefined by its very antithesis: polygenic risk scores linked to the mass of real time information collected by tech companies.17 Artificial intelligence and quantum computing will yield transformational benefits. Whether they will help us, as optimists believe, once more ‘learn how to be human’ remains to be seen.18
Covid-19 has further altered the practitioner’s gaze. The rapid transformation of practice to remote consulting has been astonishing. The limited evidence base suggests that the acceptability and effectiveness of video-consultations compare with that of traditional clinic-based care19 but few studies have been carried out in general practice. Whether the employment of new communication technologies can be employed in ways that sustain meaningful continuity of care will determine the discipline’s future.
The song remains the same
So what would George Burrows, a founding father, make of UK general practice today? He always rued the loss of independence that would have been enshrined in a new College for GPs and would be gratified by its Royal appellation. He would approve developments in training but be surprised by the disappearance of most surgery from practice. He might be permitted some schadenfreude in respect of the other Colleges and their desire to keep upstart GPs at bay. In that early disunity, he would discern the roots of the ‘independent contractor’ status that divides the NHS to this day.20 He might note wryly how little has changed in the volumes of physic that GPs prescribe and their dependence on dispensing. On the other hand, he would be astounded by the complexity of a modern practice. He would observe how their origins as tradesmen have equipped them as entrepreneurs and commissioners. Finally, he would note that doctors have always grumbled about their lot.
Constant advance characterizes biomedicine and the range of treatments available today would bemuse Burrows. Yet while many aspects of practice have greatly changed, it is more striking how little this is reflected in the day-to-day dynamics of general practice. The main business of front-line work is, as it always was, managing mental health and acute as well as chronic illness. The patients encountered by all those Drs Skrimshire and Gillam suffered from the same problems as those visiting my surgery this morning – depression, cardiac problems, minor injuries – but the landscape of health care is very different. Try to imagine practising without agreed qualifications and training standards, extended teams and purpose-built premises, managers and regulation, let alone guaranteed pay and effective remedies.
The first William Skrimshire would wonder at the strange, technological complexity of general practice today. In many respects, it is more efficient and effective. It is not obviously more responsive or personal. He would, on the other hand, recognize many of the patient-centred rhythms and rituals of practice. True, GPs now have many more complex decisions to make – which diagnostic tests to request, which medicines to prescribe, which fellow professionals to involve or refer to. The job is supposedly more stressful and demanding. Against that, fewer house calls or protracted bedside vigils are required and good pay is guaranteed. Though the cliché is well worn, clinical decision-making – the whether and how to intervene – remains art as well as science. What William’s descendants and their patients prized was continuity of care with someone they knew, a relationship of trust and dependability – always the basis of our effectiveness. We forfeit such relationships at our peril.
This article is one in a five-part series: A short history of general practice:
Professional roots https://bjgplife.com/a-short-history-of-general-practice-professional-roots/
The coming of family practice https://bjgplife.com/a-short-history-of-general-practice-the-coming-of-family-practice/
Servants of the state https://bjgplife.com/a-short-history-of-general-practice-servants-of-the-state/
Consumerist medicine https://bjgplife.com/a-short-history-of-general-practice-consumerist-medicine/
The changing gaze https://bjgplife.com/a-short-history-of-general-practice-the-changing-gaze/
References
Foucault M. The Birth of the Clinic: An Archaeology of Medical Perception. New York: Random House, 1963.
Jordanova L. The Social Construction of Medical Knowledge. Social History of Medicine 1995; 8: 361-81.
Marinker M. In Loudon I, Horder J, Webster C eds. General Practice under the National Health Service, 1948-1997. Chapter 3. ‘What is wrong’ and ‘How we know it’: Changing Concepts of Illness in General Practice. London: Clarendon Press, 1998, pp 88-9.
Loudon I. The Concept of the Family Doctor. Bulletin of the History of Medicine 1984; 58, No. 3: 347-362.
Taylor S. Good General Practice. A Report of a Survey. Oxford: Nuffield Provincial Hospitals Trust, 1954.
Royal College of General Practitioners. The Future General Practitioner: Learning and Teaching. London: RCGP, 1972.
Balint M. The doctor, his patient and the illness. London: Pitman, 1957.
Pereira Gray D, ed. Forty Years On. The Story of the First Forty Years of the Royal College of General Practitioners. London: RCGP, Atalink, 1992.
Heath I. Medicine needs an injection of humanity. BMJ 2016; 355: i5705.
Berger J. A Fortunate Man. London: Pantheon, 1967.
RCGP. Health and prevention in primary care. Report from general practice no. 18. (Chairman: J Horder.) London: Royal College of General Practitioners, 1981.
Tudor Hart J. A New Kind Of Doctor. London: Merlin Press, 1985.
Secretaries of State for Health. Working for Patients. Cm 555. London: HMSO, 1989.
Huygen F. Family Medicine: The Medical Life History of Families. Nijmegen: Dekker & Van De Vegt, 1978.
Marinker M. The Family in Medicine. Proc Royal Soc Med 1976; 69: 115-24.
Jewson N. The disappearance of the sick-man from medical cosmology, 1770-1870. Sociology 1976; 10: 225-44.
17. The Economist. Technology Quarterly. Personalised medicine. The coming of the datome. March 14th, 2020, pp 11-12. https://www.economist.com/technology-quarterly/2020/03/12/medicine-is-getting-to-grips-with-individuality
Russell, S. Reith Lecture: What will AI mean for the future of work? BBC Radio 4 – The Reith Lectures, Stuart Russell – Living With Artificial Intelligence, AI in the economy
Greenhalgh T, Wherton J, Shaw S et al. Video consultations for covid-19 BMJ 2020; 368 doi: https://doi.org/10.1136/bmj.m998
Majeed A. Should all GPs become NHS employees? BMJ 2016; 355: i5064.
Featured image by Petri Heiskanen on Unsplash
Stephen Gillam is a semi-retired GP and public health specialist who has written extensively in both fields. He is the author of ‘Of Patient Bearing – A History of General Practice in Eight Generations‘ and winner of the RCGP and Society of Apothecaries Rose Prize in the history of British general practice.
Introduction
The final generations of my family witnessed the culmination of an epidemiological transformation as well as a revolution in the means of managing it. Most striking was the shift away from acute infectious diseases to the degenerative diseases associated with ageing of the population. Henceforth, the GP’s work consisted in long-term care of chronic diseases like diabetes, in health promotion and screening. Social and economic advances were largely responsible for increasing longevity but a therapeutic revolution played its part.
The remedies available to my grandfather had been extremely limited. The thirty years from 1950 produced an explosion of therapies: e.g. vaccines, steroids, antibiotics, drugs for mental illness, cancer, heart and lung disease. Despite setbacks such as the thalidomide disaster, ‘breakthroughs’ seemed a daily media occurrence. Prescribing costs duly escalated.
The modern GP needed to absorb an enormous amount of constantly changing knowledge. Between 1959 and 1974, the number of blood tests and x-rays ordered by GPs in England and Wales rose seven-fold as hospitals opened access to these investigations. Between 1953 and 1993, outpatient attendances rose from 47 million a year to 64 million.1 The shift of care into the community was also associated with a degree of specialisation in general practice. Within partnerships, individual GPs might develop special interests in particular diseases: hypertension, asthma, diabetes, etc. The sheer volume of new knowledge represented a threat to the generalist.
The Family Doctor Charter – reversing the decline
By the early 1960s, general practice was in crisis as economic realities failed to match professional aspirations. Following a now familiar pattern, negotiations were disrupted by a bout of professional militancy over unpalatable recommendations from the pay review body. The perspicacious minister, Kenneth Robinson, intervened to avert the threat of mass resignation and broker agreement with the profession’s representatives. The resulting Family Doctor Charter was translated into a new contract in 1966. It introduced major changes to remuneration that were to have lasting effects on practice organisation and structure.2 Overall pay was increased while the proportion of capitation-based income fell relative to basic practice allowances and fees for services such as immunisation. Each doctor was reimbursed for 70% of the wage costs of up to two nursing and/or ancillary staff. An independent finance corporation to make loans for the purchase, erection and improvement of premises was set up.
These developments gradually altered the doctor’s working day. The proportion of patients visited at home halved over the same period, just as the annual number of consultations per patient rose from three to five per patient. The increasing size and complexity of practices was one reason why more practitioner time was spent on activities other than patient care – administration, meetings and training.
Beyond these changes, the Charter facilitated a subtler ideological shift. The newly instituted College helped to hasten the development of academic departments and the promotion of higher clinical and training standards. The Charter provided an indispensable material base from which to attain these standards.
By the 1980s, general practice was a self-confident discipline with a burgeoning research base and enviable training standards able to attract those from the highest rungs of Moran’s infamous career ladder.3 For many, these years are a high watermark.
Yet all was not well. Health is the capacity to cope with the existential realities of death, pain, and sickness. Modern medicine had gone far in its mission to eradicate these experiences but was falling prey to its own successes.4 General practice was struggling to deal with burdens of ‘dis-ease’ for which it was ill-equipped. Technology can often help but, in so doing, it can turn people into consumers or objects – destroying their very capacity for health. The commodification of health care was to preoccupy my generation.
Working for Patients?
In 1989, Margaret Thatcher’s government inaugurated an ‘internal market’ that separated providers of care such as hospital trusts from its purchasers of which GP fundholders proved the most agile. Sanctimonious commentators (like myself) decried these market-oriented reforms. Simultaneously, enterprising GPs exploited these opportunities to expand their services and increase their incomes. True to their shop-keeping roots, GPs displayed their customary resourcefulness. They were the fifth columnists that helped to entrench these reforms. The costs and benefits – for patients, managers and doctors themselves – are hard to compute. Arguably, these changes have diverted GPs’ energies from their core purpose.
Subsequent administrations of all hues continued their search for the holy grail: a market model that is more efficient. Governments and their ministers, despite pledges to the contrary, immersed themselves in needless structural reorganisation. Sadly, there is little substantive research evidence to demonstrate that any commissioning approach has made a significant impact on secondary care services.5 The consequences of the ill-fated Health & Social Care Act have been particularly lamentable. Given that the main policy objective of commissioning was to shape health systems around the needs of patients and shift funding from hospitals into the community, this is a disappointment.
The perils of progressivism
Medicine has never been synonymous with scientific progress. History suggests that unbridled optimism in medical science is unwarranted. Proponents of the new genetics and artificial intelligence peddle reductionist fantasies. The notion that we will ever explain and control all disease is illusory. Genuine progress is always welcome but an ideological obsession with the ‘new’ has undermined doctors’ most valuable asset: knowledge based on practical experience.
Over the last thirty years, the individualistic culture of general practice has been eroded and replaced by a management culture that threatens its traditional role.6 Rule following (guidelines and algorithms) have replaced action based on understanding. Externally imposed targets have replaced internal, personal motivations. Measurable parts (bodily systems) have distracted from indefinable wholes (people). Training has replaced education. More mandatory education leaves less room for self-directed learning. The common thread is a preoccupation with process (the ‘how’) rather than purpose (the ‘why’). The endpoint is a culture that is risk averse and unable to tolerate living with uncertainty, that attends to surface appearances rather than deeper content, to mechanism not meaning.
‘Good’ general practice
Today’s ‘crisis’ in general practice is also the result of a more fundamental, quasi-philosophical questions – as yet unresolved. What is good general practice and what is it really for? A quarter of a century ago, Peter Toon elegantly delineated three principal models of general practice: a preventive, public health approach with Hippocratic roots; a biomedical model with its basis in scientific medicine and the Enlightenment; and a humanist model (of which the Balint movement is an example) which is expressive of an older philosophical tradition.7 All three models have distinctive strengths, weaknesses and sometimes conflicting ethical foundations. For example, the utilitarian values underpinning population-oriented care are often at odds with the individualistic nature of the doctor-patient relationship.
As we have seen, from the early 1800s, general practitioners served public health functions as local medical officers superintending sanitary projects and vaccination programmes at a time when they had but a few symptomatic remedies in their armamentarium. Epidemiological enquiry has continued to break down the binary distinction of health from illness, transforming symptoms and signs into ‘risk factors’. Despite undoubted benefits, screening and other forms of health promotion have come at a cost: the medicalization of normal life. The effectiveness of preventive medicine is contested. Charged with changing behaviours they cannot control, many GPs resent responsibility for essentially political objectives.8
From the biomedical perspective, the main focus of general practice today is chronic disease management. Scientific progress has extended impressively the technological range of general practice. Information and communication technologies are continuing to transform medical knowledge and practice. However, most day-to-day practice remains, as it always has been, acute-on-chronic. Evidence-based medicine requires clinical decisions to be rooted in ‘health intelligence’ rather than the practitioner’s wisdom. The Quality and Outcomes Framework (QOF), a large pay-for-performance programme, represented a zenith in this regard. Worthily based on the latest evidence, it successfully reduced variations between practices against a basket of process indicators but, overall, over £1 billion of annual expenditure yielded little evidence of improved outcomes in population health.9
Toon’s third domain saw medicine as quintessentially concerned with human relationships. Rejecting a dualist model of personhood, the role of the doctor is (sometimes) to enhance the patient’s coping abilities and promote acceptance of illness as meaningful. For much of what presents in general practice cannot simply be suppressed or removed. The goal of care then is psychological adjustment and understanding.
Foremost among contemporary commentators, Iona Heath writes eloquently of the need to recalibrate consultations with more emphasis on those aspects for which evidence-based medicine (EBM) has no answers.10 Scientific reductionism devalues individual experience. While EBM describes people in terms of biomedical data, clinicians must interpret more complex information to help individuals make sense of their illness – and do so under conditions of uncertainty.
For many practitioners, the language of this humanist domain is abstruse. The work of Michael Balint on the psychodynamics of the doctor-patient relationship is no longer central to the training of general practitioners. Too much emphasis on such soft skills can cloak technical failings. Anyway, the argument goes, continuity of care is less important for younger users meeting all their informational needs from their smartphones. But for those less scientifically literate, e-medicine can be a source of confusion and vulnerability. Their priorities may be subservient to those of medical-industrial interests.
Ironically, it is this third domain that underpins general practitioners’ ability to deliver both effective prevention and efficient technical care. It is facilitated by – and sometimes conflated with – continuity of personal care. Despite evidence that such continuity may be associated with reduced mortality11, policy makers continue to prioritize access. Practitioners recognize this domain as it comprises much of their everyday. Biomedicine is positively unhelpful in promoting the delusion that ‘something (technical) can be done’ for many conditions. AI is not going to displace the doctor as drug any time soon. Rather, personal contact with a known and trusted source of support will become ever more precious.
Toon’s typology (here simplified) helps to map our professional territory. Having analysed the philosophical concepts underlying his paper’s title, Toon’s conclusions were deceptively simple. He noted two fundamentally different aims of general practice: hedonic (helping patients avoid suffering) and hermeneutic (concerned with patients’ search for meaning). He regretted the absence of a theory of justice properly able to reconcile these different aims.
Conclusion
Health systems are part of the fabric of social and civic life. They both signal and enforce societal norms through the personal experiences of providers and users. These norms may indirectly be as salutogenic as the technologies provided. Practices of themselves generate social capital within their communities. Direct experience is what will shape future support for general practice too. However, workforce trajectories suggest that ‘relationship-based care’ may soon be nurse-led or the preserve of the affluent.
There is much from which to take pride and confidence today – for example, around training, organization and quality of care. Yet it hardly needs restating that general practice faces an uncertain future. Pickstone has argued that the NHS typified a communitarian approach to medicine, characterised by social solidarity, in contrast to the productionist model that preceded it and the consumerist medicine that prevails today.
Unwitting consumers are helping to drive overdiagnosis and overtreatment, most of it futile, wasteful, and damaging to patients, and all compounded by a significant environmental impact. These harms are driven by the desire to exploit disease for profit and threaten the financial viability of healthcare systems.
Iona Heath invokes the concept of ‘rewilding’ as a metaphor for restoring the delicate ecosystem of general practice. Only a strong system of primary healthcare underpinned by a commitment to social justice and built on long-term, trusting relationships has the power to resist repeated waves of exploitation by commercial interests and politicians. It is a plea that my forbears would have endorsed.
This article is one in a five-part series: A short history of general practice:
Professional roots https://bjgplife.com/a-short-history-of-general-practice-professional-roots/
The coming of family practice https://bjgplife.com/a-short-history-of-general-practice-the-coming-of-family-practice/
Servants of the state https://bjgplife.com/a-short-history-of-general-practice-servants-of-the-state/
Consumerist medicine https://bjgplife.com/a-short-history-of-general-practice-consumerist-medicine/
The changing gaze https://bjgplife.com/a-short-history-of-general-practice-the-changing-gaze/
References
Rivett G. From Cradle to Grave. Fifty years of the NHS. London: King’s Fund, 1998.
The Family Doctor Charter. London: HMSO, 1966.
Curwen M. Lord Moran’s Ladder: a study of motivation in the choice of general practice as a career. J Coll Gen Pract 1964; 7: 38-64.
Le Fanu J. The Rise and Fall of Modern Medicine. London: Abacus, 2011.
Smith J, Mays N. GP led commissioning: time for a cool appraisal. BMJ 2012; 344: e980.
Willis J. The Paradox of Progress. Oxford: Radcliffe Medical Press, 1995.
Toon P. What is Good General Practice. Occasional Paper 65. London: Royal College of General Practitioners, 1994.
Fitzpatrick M. The Tyranny of Health. London: Routledge, 2001.
Ryan AM, Krinsky S, Kontopantelis E, Doran T. Long-term evidence for the effect of pay-for-performance in primary care on mortality in the UK: a population study. Lancet 2016; 388: 268-74.
Heath I. The Mystery of General Practice. London: Nuffield Provincial Hospitals Trust, 1995.
Pereira-Gray D, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors-a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open 2018, 8, 6.
Heath I. Rewilding general practice. British Journal of General Practice 2021; 71 (713): 532-533. DOI: https://doi.org/10.3399/bjgp21X717689
Featured image by Hush Naidoo Jade Photography on Unsplash
Stephen Gillam is a semi-retired GP and public health specialist who has written extensively in both fields. He is the author of ‘Of Patient Bearing – A History of General Practice in Eight Generations‘ and winner of the RCGP and Society of Apothecaries Rose Prize in the history of British General Practice.
Introduction
My great great great grand-father George Skrimshire (1802-1877) represented the third generation of generalists. He joined his uncle William as an apprentice in Wisbech. In his deed of indenture, George forswore ‘fornicating…matrimony contract, Taverns, Inns or Alehouses… Cards, Dice, Tables or any other unlawful games… His said Masters the said Apprentice in the Art of Surgery and Pharmacy which they now useth shall teach and instruct during the said term of five years.’ Training already involved the instillation of a more professional ethos.
On March 31st 1823, he received his Certificate of Satisfactory Apprenticeship, ‘having conducted himself with great proficiency and as far as respects his moral conduct entirely to (their) satisfaction.’ He then moved to London, to ‘walk the wards’ at Guy’s Hospital and prepare for his Licentiate of the Society of Apothecaries.
In 1841, George moved to Norfolk, and the house where I live now. He worked hard to establish his practice. Whether Holt was well chosen for the medical opportunities it presented is open to question. There was no lack of competition and his wife Lavinia wrote of ‘a very sad first year, no sickness scarcely at all’. Together they were there to rear 13 children of whom four went into medicine.
Rising status, falling self-esteem
Many doctors in the early nineteenth century felt they were held in low regard by a public happy to employ the practitioner charging the lowest fee. Status came to rest on acquired standards of behaviour rather than superior knowledge. Peterson describes a ‘social chasm’ between medicine and other ‘liberal professions.’1 Less than 20% of practitioners came from the families of gentry or other non-medical professionals. Historians are less harsh. ‘The lawyer and the doctor took the lead amongst the middle classes of Middlemarch, or in the suburbs of London…’2 For in the first half of the nineteenth century, specialisation had not yet become the pathway to prosperity or high status.
Why then did these reliable all-rounders not establish themselves as equals? In large part, it was because the practice of pharmacy was a reminder of their original trade and the apothecary’s shop. It blurred their distinction from the reviled druggist. Then as now, many GPs felt that to become a respectable member of the medical profession, they would have to abandon pharmacy while others defended the right to dispense as a skill best performed by one with a medical education and the opportunity to observe the effects of their actions.
The social insecurity of the GP was aggravated by continuing acrimony within the profession. ‘The way things are constituted the general practitioner finds himself treated rather as a tradesman than a gentleman.’3 Some of this disdain lingers today in the commonplace perception of GPs as financially motivated businessmen by comparison with their supposedly more altruistic consultant colleagues.
GP Income
Private practice was the main source. Although reliable data are limited, between 1780 and 1820 doctors improved their financial position to a greater extent than other groups.4 Thereafter, it declined due to overcrowding and market forces. Like students today, they were under early pressure. Between 1815 and 1850, around £1000 (four years’ income) was needed to cover an apprenticeship.33 An 1842 guide to parents reminded them that ‘by the time when a physician earns his bread and cheese he has no longer the teeth to eat them with.’5
George and his successors derived income as vaccinators and school doctors. Their most important additional appointments were as ‘parish surgeons’ before and ‘union surgeons’ following the Poor Law Amendment Act of 1834. As union surgeons, they were paid less for looking after larger numbers of sick poor. The status of medical officer was thus degraded and GPs suffered financially as a consequence. From the average salary of £69 per annum practitioners had to provide drugs and dressings.6
Overall, GP incomes therefore changed little between 1820 and 1850. Indeed, taking the costs of living into account, the Eighteenth century surgeon apothecary was more prosperous. A minimum of £200/year was needed for a way of life that included domestic servants, private education for children, the necessary standards of house, furniture and dress. Most commonly, income during this period was between £150-200 in the country, £300-500 in larger towns.
The relative sparsity of data raises the suspicion of deliberate concealment. Income tax was re-imposed by Robert Peel in 1842 for incomes over £150 and this may have prompted reticence. GPs came under schedule D and could deduct all expenses incurred in the course of work. Creative accounting has always been a useful skill in general practice.
If real incomes were lower in mid-century, buying into a successful practice or succeeding father or uncle was the surest route to prosperity. More than half the population and more than half of all GPs lived in rural areas. Country practice was generally less well paid. GPs therefore often hovered for years on bare subsistence.
Public approbation
An Act to Regulate the Qualifications of Practitioners in Medicine and Surgery was finally passed in 1858. This established the General Medical Council, a medical register and forever reified the distinction between physicians, surgeons and general practitioners. The latter thereafter acquired exclusive rights of referral to hospital specialists and their role as ‘gatekeepers’. In the oft-quoted aphorism: ‘The physician and surgeon retained the hospital but the GP retained the patient.’7
The extent to which regulation benefited patients is disputed but doctors consolidated their professional monopoly. Yet in one respect the Medical Act resembled the 1815 Apothecaries Act: to the majority of practitioners it was a disappointment as it failed to wholly outlaw quackery.
The second half of the nineteenth century saw the emergence of the ‘family doctor’. The fictional stereotype was often poor, shabby and old-fashioned, but always accessible and enjoying the confidence of his patients. A users’ guide indeed intoned: ‘Let not your doctor be too useful…and avoid the man whose dress and demeanour indicate puppyism… Be not averse to him if he is slovenly in apparel.’8 The ideal of the family doctor was enormously powerful in shaping public and professional perceptions of contemporary practice. It provided GPs with a new corporate identity – as neither business-like apothecaries nor impassive physicians. In Loved at Last, the GP Mr Gregory ‘bore with noble courage and patient bearing…broken rest… long rides…exercising a skill and knowledge acquired by years of study and acute observation.’9
The GP was expected to sit patiently at the bedside through long hours and to deal with any emergency at any time of day or night. As George’s father wrote to him in 1830: ‘When the stormy winds are blowing and the rain is battering against our windows, often does your mother exclaim, I wonder whether poor George is riding about on this dark and dreary night. When we are sitting round our social fire your sisters observe you are wanting to make up the circle and to join in with your flute in the harmony of the evening.’
The role was a demanding one in other ways. Poverty, competition, the costs of education and establishing a practice were recurrent concerns for practitioners. More corrosive were the emotional and spiritual challenges of the work – the relentless grind of never-ending demands, the exhausting affront of patients’ poverty, and hopelessness in the face of incurable illness. Professional isolation was extreme.
Medical education
As we have seen, until the 1830s medicine was still largely based on Greek and Roman ideas. Little was known of the causes of disease. Enquiring doctors, without university training, looked for explanation by studying natural history and science. Medical studies were more formally structured after 1858 following GMC guidelines. Potential medical students were required to take a preliminary exam to demonstrate liberal educational attainment followed by a minimum of five years in training. Practice was proscribed before the age of 21. Two or three years of pre-clinical studies were followed by three or four years of clinical training, very much as now.
To this day, there is continuing debate over the most appropriate sequencing and balance of theoretical versus practical work, and how to accommodate new sciences. There were concerns that factual cramming restricted their outlook. ‘There is…no profession in which it is more essential that those engaged in it should cultivate the talent of observing, thinking and reasoning for themselves, than it is in ours. You have done not much more than learn the way of learning. The most important part of your education remains.’10 The education of GPs has always been vitiated by the needs of specialists. Students often gained more experience of ‘serious’ (rare) illness in hospital rather than common conditions found in the community.
The recognition of what are nowadays called ‘consultation skills’ date from this period. A good bedside manner was seen as financially expedient too. A liberal education would fashion the interpersonal skills suitable for a gentleman and facilitate communication with more affluent patients.
The expansion of hospital-based training in the nineteenth century helped to improve the image of medicine – and parental willingness to pay for it. Though some students may have been coarse and lazy (think Dickens’ Ben Allen and Bob Sawyer), most were well-mannered and conscientious. Then as now, there were the initiations of dissecting room and theatre – experiences that toughened the emotional carapace for the rigors of the job.
Key questions for educationalists concerned the character of pre-clinical education, the location of training, curricular content, the relationship of surgery to physic, the place of anatomy and dissection, and the relationship of bedside medicine to experimental science. A century and a half on, we wrestle with the same dilemmas but the roots of present educational practice were firmly in place by the middle of the nineteenth century.
Conclusion
General practitioners failed to achieve parity with physicians and surgeons for multiple reasons. Voluntary hospitals dominated medical education and general practitioners were entirely divorced from teaching. Their leaders were constantly outflanked by the persistent obstructionism of the Physicians and Surgeons. Many of these barriers persisted till the recent past.
The Medical Act is hailed both as a landmark through which the profession put its house in order and as a prime example of monopolization. From this time dates the second of the three pillars of modern-day general practice – the concept of referral rights. The first was the notion of generalism itself; the third being the registered list which emerged early in the next century.
George died in 1877 leaving for his son John Truscott Skrimshire (1835-1912) the prerequisites of prosperity: 15-20 visits/day, an efficient pharmacy run by his apprentice or assistant, the minimum of bad debts and a prominent house on the highway. Traditional person-centred medicine had derived its authority as much from social as from clinical skills. These ‘arts’, always vigorously defended,11 were henceforth combined in the exercise of scientific medicine and a resurgent professionalism. However, general practice remained a wearying and dangerous occupation as we shall see.
This article is one in a five-part series: A short history of general practice:
Professional roots https://bjgplife.com/a-short-history-of-general-practice-professional-roots/
The coming of family practice https://bjgplife.com/a-short-history-of-general-practice-the-coming-of-family-practice/
Servants of the state https://bjgplife.com/a-short-history-of-general-practice-servants-of-the-state/
Consumerist medicine https://bjgplife.com/a-short-history-of-general-practice-consumerist-medicine/
The changing gaze https://bjgplife.com/a-short-history-of-general-practice-the-changing-gaze/
References
Peterson M. Gentlemen and Medical Men: the Problem of Professional Recruitment. Bulletin of the History of Medicine 1984: 58; 457-73.
Reader W. Professional Men. London: 1966, p 68.
Medical Education and Rank. London Medical Repository 1820; 14: 123-9.
Lindert PH, Williamson JG. English workers’ living standards during the Industrial Revolution. Economic History Review 1983; 36: 1.
Hudson JC. The Parent’s Handbook. London, 1842.
Griffin R. Grievances of the Poor Law Medical Officers. London, 1859.
Stevens R. Medical Practice in Modern England. New Haven: Yale University Press, 1966.
Hints on Choosing a Doctor. A Penny Magazine 1832; 1: 309-10.
Lemon M. Loved at Last, 3 vols. London: Bradbury & Evans, 1864, i, 8.
An introductory discourse on the Duties and Conduct of Medical Students and Practitioners. 1843, 15-17.
Lawrence C. Incommunicable Knowledge. Science, Technology and the Clinical Art in Britain, 1850-1914. J Contemporary History 1985; 20: 517.
Featured image: Three children automatically putting out their tongues for inspection upon meeting the family doctor in Kensington Gardens. Wood engraving after J. Leech, 1861.. Credit: Wellcome Collection. Public Domain Mark
Stephen Gillam is a semi-retired GP and public health specialist who has written extensively in both fields. He is the author of ‘Of Patient Bearing – A History of General Practice in Eight Generations.’
Introduction
I was 47 years old when I discovered, almost by accident, that I was eighth in a line of generalist doctors dating back to 1770. It was something of a shock. Most of us like to believe we exercise free will and discretion over our life choices. Mine it seemed had been determined two centuries earlier. Doctors are inclined to be fatalistic for we witness every day the impact of genes and inheritance on our patients’ lives. However, I was left pondering my ancestors: their lives and livelihoods, their foibles, strengths and flaws – and their influence on mine.
My book tells the story of general practice down those eight generations.1 It describes the evolution of the discipline from its apothecary roots, focusing on themes such as the burden of disease, developments in policy, practice, training, pay and conditions.
Talking to medical students, registrars and even peers, I am forcibly struck by how little they know of our history. The commonest misconception is that general practice, the ‘jewel in its crown’, is largely a product of the NHS. This short series of articles hopes to inform, stimulate and provoke.
From Apothecary…
My family’s origins were humble. The surgeon-apothecary William Skrimshire (the Older) (1739-1814) practised in the marshy hamlets and villages around Wisbech. In those days, malaria and other marsh fevers were still a scourge. A plurality of practitioners offered their services2 in the 18th century medical marketplace. The profession of apothecary can be dated back to Babylonian times. GPs today may offer many of his services but the modern pharmacist is the apothecary’s more obvious descendent. The Worshipful Society of Apothecaries, founded in 1617 admits members by examination to this day.
The period from around 1790 to 1860 yielded major medical reforms in Britain.3 In William’s time there was not one medical profession but three. The physicians, members of a learned profession, dealt with internal disorders. Surgeons were craftsmen whose sphere was still largely external. Apothecaries compounded and dispensed physicians’ prescriptions until they won the right to visit, advise and prescribe (see below). This well-known division conceals the extent to which their respective practices overlapped with one another – and those of many untrained, less costly ‘irregulars’ (travelling quacks and charlatans).
The traditional view of rank-and-file practitioners such as William characterizes them as ill-educated and near-illiterate tradesmen who kept shops selling medicines and groceries to supplement earnings from their primitive practice. This caricature is harsh. In addition to dispensing medicines directly to patients, the apothecary offered general medical advice and a range of services that are now performed by other specialist practitioners, such as surgeons and obstetricians. Apothecaries often operated through a retail shop which, in addition to ingredients for medicines, sold tobacco and patent medicines. They were, in other words, frequently the sick person’s point of first contact.
Much had changed on 15th March, 1704 when William Rose was prosecuted for treating William Seale, a butcher at Hungerford Market. Annoyed at his £50 bill, Seale had sought redress through the College of Physicians. Lord Chief Justice Holt reluctantly found in favour of the College on a point of law but the House of Lords sensibly reversed the judgement in the light of customary practice.4 Much has been attributed to this infamous case including our present-day tendency to over-prescribe. Its impact on the status of apothecaries was ambiguous. On the one hand, the decision perpetuated their inferior status as financially dependent on sales of goods rather than expert knowledge. On the other hand, apothecaries were free to practice physic and become the doctors of the poorer classes. It gave legal confirmation for the first time to their role as medical practitioners rather than tradesmen.
The rise of the surgeon-apothecary in the eighteenth century was in large measure driven by economic expediency. Most surgeons practiced physic and pharmacy in order to survive while apothecaries frequently undertook simple surgical procedures. Across the country in small towns and villages, most medical men – however they styled themselves – were undertaking much the same kind of general practice, involving all branches of medicine.
…to General Practitioner
William’s son, another William (1766-1829), was the first to qualify as a doctor but his passion was entomology. He bequeathed an extensive herbarium to the Wisbech museum. He was the first to write of using roasted iris seeds as a coffee substitute5 and was entrepreneurial too. He concocted a product called ‘British Salop…as a substitute for cocoa, chocolate, tea and coffee…one of the most nutritious preparations ever offered to the public…as useful in the sick chamber as at the breakfast table.’ This, after all, was the ‘Golden Age of Physic’.6 To this day, a taint of trade lingers about our branch of the profession.
Medical education then was a thriving industry but chaotic. Organised training and qualifications did not distinguish regulars from irregulars. Aspiring doctors’ increased financial expectations were some compensation for the initial outlay but their livelihoods were threatened still. Pressure for reform was growing up from below.
A major driver for change was thus the rise of dispensing druggists. Like many apothecaries before them, they served their apprenticeships as grocers or tea dealers but observed the profits to be made from pharmacy. A striking feature of proto-GPs’ surviving accounts and workbooks is the vast quantities of medicines dispensed and their financial dependence on prescribing.7 By 1794, surgeon-apothecaries were each now losing £200/year to druggists.
Dr Edward Barlow was foremost among those with proposals to transform ‘that excellent species of practitioner, the surgeon-apothecary’ into an educated generalist. ‘On the competency of this class must the great mass of the population rely for the preservation of health and removal of disease. To by far the greatest portion of society they are the sole physicians, and even the highest ranks are known to depend with fullest confidence on their skills and ability.’8 Barlow’s particular concern was the chaotic state of medical education. He believed the College of Surgeons was the most appropriate institution to take on responsibility for training and oversight.
The first association properly to address the needs of general practitioners was founded – in the best professional traditions – at a meeting in the Crown and Anchor in the Strand on 3rd July, 1812. A protest had been called in response to a rise in tax on glass by which apothecaries had been hard hit. A new Association of Apothecaries and Surgeon-Apothecaries of England and Wales was proposed. Its object was to improve the education and status of the profession. Its indefatigable chairman, George Man Burrows (1771-1847), has been called the ‘father of general practice’.9
With great perseverance Burrows led the production of a Bill that combined idealism and self-interest. The Association’s aims were, firstly, improved training and examination based on a broad curriculum and, secondly, a licensing process that clearly distinguished irregular practitioners from the formally educated. It proposed that future general practitioners be examined and licensed by a ‘fourth body’, that they be required to hold a diploma from the Royal College of Surgeons and that a new London-based school of medicine be founded for their training. In this manner, the surgeon-apothecary would gain legal status as a generalist licensed in medicine, surgery and midwifery while unlicensed practitioners would be liable to prosecution. The idea of a fourth body (or College of General Practitioners) was, of course, anathema to the other Colleges and duly suppressed.
The Apothecaries Act had received its first reading on January and was eventually passed by the House on 11 July, 1815. The Society of Apothecaries was to be responsible for the examination and licensing of future general practitioners and for prosecuting the unlicensed. Candidates for the Licentiate of the Society of Apothecaries (LSA) were required to have spent six months at a recognized hospital or dispensary. The penalty for practising without a licence was £20 but ‘Pre-1815’ medical men were exempted. Membership of the Royal Society of Surgeons (MRCS) was not compulsory but the diploma was so frequently taken that the dual qualification MRCS LSA (colloquially known as ‘College and Hall’) became our hallmark.
On the one hand, the Act added compulsion and examination to the pre-existing educational framework and was a step forward towards full professionalization. The term ‘medically qualified’ at last had a clear meaning. On the other hand, the Act was undoubtedly muddled with no clear definition of an apothecary or what constituted illegal practice. It failed to outlaw irregulars.
Conclusion
Was the Apothecaries Act among the great reforms of the nineteenth century or a degrading compromise in the face of reactionary opposition from the Colleges of Physicians and Surgeons? Medical historians are divided. Few general practitioners were satisfied with the outcome but GP numbers nevertheless grew rapidly over the first decades of the nineteenth century.
The GP was thus not a sudden creation but evolved from the surgeon-apothecary and man-midwife in the first half of the eighteenth century. This evolution was as much a product of political struggle as of planned progress in medical education and practice. No history can ignore the dubious consequences of GP exceptionalism which surely dates back to these early struggles. Down the decades, GPs have generally never had it so bad: battling threats real or imagined from less qualified competitors, countering the condescension of Royal Colleges, or fighting off managerial incursions. Shroud waving is a tribal pastime. Bouts of professional militancy went on to feature in the early days of national health insurance and the NHS. They continue to shape the profession’s self-image to this day. A necessary part of the practitioner’s armamentarium has always been the ability to subvert official controls.
The term ‘general practitioner’ was slow to catch on with the general public but by the middle of the nineteenth century, it was in common use among a confident new medical cadre with a growing sense of corporate identity.10 William Skrimshire (the Younger) ended his working days as one-such doctor.
This article is one in a five-part series: A short history of general practice:
Professional roots https://bjgplife.com/a-short-history-of-general-practice-professional-roots/
The coming of family practice https://bjgplife.com/a-short-history-of-general-practice-the-coming-of-family-practice/
Servants of the state https://bjgplife.com/a-short-history-of-general-practice-servants-of-the-state/
Consumerist medicine https://bjgplife.com/a-short-history-of-general-practice-consumerist-medicine/
The changing gaze https://bjgplife.com/a-short-history-of-general-practice-the-changing-gaze/
References
Gillam S. Of Patient Bearing – A History of General Practice in Eight Generations. Holt: Hill House Publishing, 2021.
De Renzi S. The Sick and their Healers. Chapter 2 in Elmer P ed. The Healing Arts. Health, Disease and Society in Europe. Manchester: Manchester University Press, 2004, pp 136-165.
Loudon I. Medical Care and the General Practitioner, 1750-1850. Oxford: Clarendon Press, 1986.
Clark G. A History of the Royal College of Physicians of London. London: RCP, 1966, pp 476-9.
Skrimshire W. Account of a British vegetable product [Iris pseudacorus], that may be substituted for coffee. Nicholson’s J Natural Philosophy 1809; 22: 70-73.
Eyre-Brooke AL. Richard Smith junior and his Life and Times. Bristol Medical Chirurgical Journal 1969; 84, 1.
Baine B. Bill from Mr Bernard Baine, surgeon apothecary to Thomas Carew. Somerset CRO, Taunton, DD/TB box 14/20, 1755.
Barlow E. A Disinterested Physician. MPJ 1813, 30, 265-296.
Bettany GT. Burrows, George Man. In Stephen, Leslie. Dictionary of National Biography. London: Smith, Elder & Co, 1886.
Bloor DU. The Rise of the General Practitioner in the Nineteenth Century. J Roy Coll Gen Pract 1978; 28: 288-91.
Featured image: The dance of death: the apothecary. Coloured aquatint after T. Rowlandson, 1816.. Credit: Wellcome Collection. Public Domain Mark