Stevie Lewis is a campaigner and board member of the International Institute for Psychiatric Drug Withdrawal. She took an SSRI for 17 years, the majority of which was spent trying and failing to stop because the withdrawal effects were so severe.
Mark Horowitz is a Clinical Research Fellow in psychiatry at University College London and North East London NHS Foundation Trust. He has a PhD in the neurobiology of antidepressants from the Institute of Psychiatry, Psychology and Neuroscience at King’s College London. He has published articles on safe tapering in Lancet Psychiatry and authored the Royal College of Psychiatry guidance on stopping antidepressants. He has lived experience of this process.
Long-awaited National Institute for Health and Care Excellence (NICE) guidance on how to safely stop antidepressants (and other drugs associated with dependence and withdrawal) were published on 20 April 20221 and outline a method of stopping antidepressants that is a sharp departure from previous guidance, based on the latest science and clinical experience in this field.2,3
While this guidance represents a significant advancement, the novelty of the guidance and the brief fashion in which it is outlined make it challenging for GPs to implement it in practice. This is why we have made a 1-hour training video to explain the details of how to safely taper antidepressants, which will allow GPs to convert this guidance into improved clinical care.4
In recent years there have been complaints from patients that the withdrawal symptoms that occur when reducing or stopping antidepressant medication are more common, severe, and long-lasting than official guidelines had hitherto indicated.5
… 17 placebo-controlled trials demonstrated physiological withdrawal symptoms from antidepressants …
In 2017, this led to the Minister for Public Health and Primary Care to commission Public Health England (PHE) to identify the scale of problems with prescribed drug dependence, including antidepressants. The PHE report6 found that 17 placebo-controlled trials demonstrated physiological withdrawal symptoms from antidepressants including insomnia, depression, suicidal ideation, and physical symptoms.
A systematic review found that these symptoms occurred in about half of patients in randomised controlled trials and that up to half of these patients reported these symptoms were severe in surveys. These symptoms could last for months or longer and cause significant effects on patients’ wellbeing and their personal, social, and occupational functioning.5,7,8
This report led to an update to the NICE guideline, which now recognises that withdrawal symptoms can last for ‘months or more’ and can be ‘more severe for some patients’ than previously recognised.1
Additionally, PHE found that patients reported that there was a lack of information on the risks of medication and a lack of acknowledgement of withdrawal effects from doctors. Patients reported that there was a lack of access to effective management and NHS support services.
As a consequence many patients have exited mainstream health services and seek advice on Facebook groups or peer-led online support communities, with surveys of these patients reporting that they found the advice gained there more useful than from the health service (Horowitz MA, unpublished data, 2022). These patients report that doctors routinely mis-interpret their withdrawal symptoms as relapse of an underlying condition.9
One of the recommendations from PHE was for improved clinical guidance on how to safely stop antidepressants. The NICE committee set up to fulfil this task have just published guidance titled Medicines associated with dependence or withdrawal symptoms: safe prescribing and withdrawal management for adults.1
… many patients have exited mainstream health services and seek advice on Facebook groups or peer-led online support communities …
This initiative has been welcomed by patients and doctors, as it replaces earlier guidance on how to stop antidepressants that was not supported by evidence. Previous guidance, which suggested ‘when stopping an antidepressant, gradually reduce the dose, normally over a 4-week period’, was not based on research evidence but based on the interpretation of the committee at the time that 4 weeks was a suitable period (after a single study showing that stopping over 1 day caused unacceptably high levels of withdrawal effects).
Instead, the new NICE guidance outlines the approach to reducing antidepressants, recommending ‘a slow, stepwise rate of reduction proportionate to the existing dose, so that decrements become smaller as the dose is lowered’.1 This will be unfamiliar advice to many GPs, and although the NICE advice represents a significant advancement in the field, the novelty of the advice and the brevity with which it is presented will leave many GPs eager to improve their practice scratching their heads.
Guidance on stopping antidepressants published by the Royal College of Psychiatrists adds useful detail to the approach presented by NICE, as well as some specific examples of dose reduction regimes.10
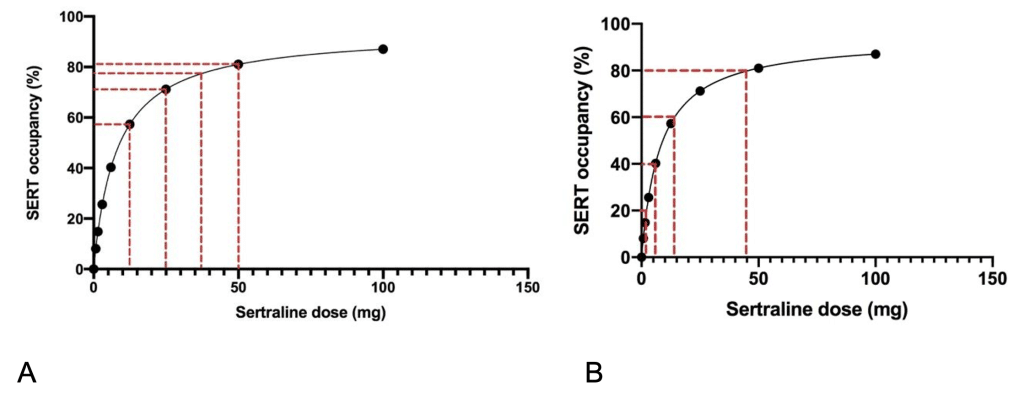
For example, in the new NICE guidelines, the recommendation to reduce dose in a proportionate manner means that the dose should be reduced by a proportion of the most recent dose. This recommendation is based on the way in which these drugs effect the brain: the relationship between dose of antidepressant and effect on the brain is very steep for small doses and flattens out at commonly used doses.2
For example, reduction of sertraline by 20% dose reductions would involve the following reductions: 50 mg, 40 mg, 32 mg, 25.6 mg, 20.5 mg, 16.4 mg, 13.1 mg, 10.5 mg, 8.4 mg, 6.7 mg, 5.4 mg, 4.3 mg, 3.4 mg, 2.7 mg, 2.2 mg, 1.8 mg, 1.4 mg, 1.1 mg, 0.9 mg, 0.7 mg, 0.6 mg, 0.5 mg, 0 mg (see Figure 1). In order to make up these doses, a liquid version of sertraline will be required or specially formulated small-dose tablets (for example, ‘tapering strips’). The increased cost of these measures in the short term is likely to lead to long-term savings in reduced prescriptions, as well as a reduction in adverse effects for patients.
In order to provide further detail on the guidance to be published by NICE, which will enable GPs to apply this guidance in practice, the International Institute for Psychiatric Drug Withdrawal, an institute founded by patients, psychiatrists, and scientists in order to advance the field of safe, patient-centred approaches to stopping psychiatric medication, has produced a training video, presented by the authors of this article.
In the video we:
• give an example of the impact on stopping antidepressants inexpertly for one woman;
• outline the evidence for previous guidance on how antidepressants should be stopped;
• distinguish between the concepts of physical dependence and addiction;
• outline the latest science on tapering antidepressants, including hyperbolic (or proportionate) tapering;
• outline how to taper antidepressants gradually in practice, including specific examples;
• outline options for making up the small doses of antidepressant required for this process; and
• summarise key tips and tricks for tapering (such as never skipping doses to taper, except for fluoxetine).
We present this video in the hope that more patients will be helped to come off their antidepressants, when it is appropriate, in a manner which is safe and effective and thus spare them from the difficulties this process can involve.
References
1. National Institute for Health and Care Excellence. Medicines associated with dependence or withdrawal symptoms: safe prescribing and withdrawal management for adults. NG215. 2022. https://www.nice.org.uk/guidance/ng215 (accessed 28 Apr 2022).
2. Horowitz MA, Taylor D. Tapering of SSRI treatment to mitigate withdrawal symptoms. Lancet Psychiatry 2019; 6(6): 538–546.
3. Framer A. What I have learnt from helping thousands of people taper off psychotropic medications. Ther Adv Psychopharmacol 2021; 11: 2045125321991274.
4. Institute for Psychiatric Drug Withdrawal. Antidepressant withdrawal syndrome and its management. 2022. https://www.youtube.com/watch?v=PSjYH044-2Q (accessed 4 May 2022).
5. Guy A, Brown M, Lewis S, Horowitz M. The ‘patient voice’: patients who experience antidepressant withdrawal symptoms are often dismissed, or misdiagnosed with relapse, or a new medical condition. Ther Adv Psychopharmacol 2020; 10: 2045125320967183.
6. Taylor S, Annand F, Burkinshaw P, et al. Dependence and withdrawal associated with some prescribed medicines: an evidence review. 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/940255/PHE_PMR_report_Dec2020.pdf (accessed 28 Apr 2022).
7. Davies J, Read J. A systematic review into the incidence, severity and duration of antidepressant withdrawal effects: are guidelines evidence-based? Addict Behav 2019; 97: 111–121.
8. Hengartner MP, Schulthess L, Sorensen A, Framer A. Protracted withdrawal syndrome after stopping antidepressants: a descriptive quantitative analysis of consumer narratives from a large internet forum. Ther Adv Psychopharmacol 2020; 10: 2045125320980573.
9. White E, Read J, Julo S. The role of Facebook groups in the management and raising of awareness of antidepressant withdrawal: is social media filling the void left by health services? Ther Adv Psychopharmacol 2021; 11: 2045125320981174.
10. Royal College of Psychiatrists. Stopping antidepressants. https://www.rcpsych.ac.uk/mental-health/treatments-and-wellbeing/stopping-antidepressants (accessed 4 May 2022).
Featured photo by Nastya Dulhiier on Unsplash.



Stevie Lewis is a campaigner and board member of IIPDW. She took an SSRI for 17 years, the majority of which was spent trying and failing to stop because the withdrawal effects were so severe.
Mark Horowitz is an Associate of IIPDW, a Clinical Research Fellow in psychiatry at University College London and North East London NHS Foundation Trust. He has a PhD in the neurobiology of antidepressants from the Institute of Psychiatry, Psychology and Neuroscience at King’s College London. He has published articles on safe tapering in Lancet Psychiatry and authored the Royal College of Psychiatry guidance on stopping antidepressants. He has lived experience of this process.
Together with IIPDW they have created a 1-hour training video to support prescribers and patients to manage antidepressant withdrawal syndrome in clinical practice. You can watch the video on our website here.
This video coincides in the UK with the long-awaited National Institute for Health and Care Excellence (NICE) guidance on how to safely stop antidepressants (and other drugs associated with dependence and withdrawal) which were published on 20th April 2022 and outline a method of stopping antidepressants that is a sharp departure from previous guidance. While this guidance represents a significant advancement, the brief fashion in which it is outlined makes it challenging for clinicians to implement in practice. The video helps provide more detail on the process of supporting a patient to withdraw from antidepressants.
The video has already been featured in an article in the BJGP Life, part of the British Journal of General Practice.
This video was supported by a funding grant from Open Excellence, and the production was by MindWick.
[…] Article→ […]
An important new book is available – for patients and prescribers – written expressly to enable better ‘informed consent’.
This is Antidepressed by Beverley Thomson, published by Hatherleigh press.
Reviewed here by Stevie Lewis:
Review of Beverley Thomson’s book ‘Antidepressed’ by Stevie Lewis, IIPDW Board Member –
Antidepressed: A Breakthrough Examination of Epidemic Antidepressant Harm and Dependence eBook : Thomson, Beverley: Amazon.co.uk: Books