 Roger Jones is Emeritus Professor of General Practice, Kings College London and the previous Editor of BJGP.
Roger Jones is Emeritus Professor of General Practice, Kings College London and the previous Editor of BJGP.
Charlotte Williamson is able to write with considerable authority on the rise of the patient movement. She has been the vice-chair of a Health Authority, chair of the patient liaison group for the Royal College of General Practitioners and helped to found patient liaison groups at the Royal College of Pathologists and the Royal College of Anaesthetists. In 2010 she published Towards the Emancipation of Patients, which traced the rise of the patient movement and described the theoretical and socio-political background to the idea of patient emancipation. In her recent book she draws on the experience of patients and patient groups, as well as changes in the professional and healthcare landscape in the UK and US to review the meaning and implications of patient emancipation and to trace the origins of the movement, and the development of the ideas and principles, that have guided it.
This book provides a more nuanced account of the problems that patients, managers and clinicians may face in creating genuine therapeutic partnerships, recognising that a hidden political agenda can subtly Influence the power relationships between them, and undermine their best intentions. Her final chapter ends with “hope for eventual equality of esteem, of voice, and of power between patients, doctors and managers. Equality is the end sought by the patient’s emancipation movement, however far away it seems “.
Reading this book, I couldn’t help reflecting on my own experiences as a clinician, a researcher, and a patient. I look back on thousands of general practice consultations in which the main challenge was to figure out exactly what had brought the patient to the surgery, and how to make sense of problems and symptoms that never appeared in the textbooks.
Working with patients on research projects concerning common gastrointestinal problems, completely new perspectives, and reports of unsuspected “lived experiences“ frequently emerged. My department at King’s hosted the first “Concordance Unit, in which prescribing and medicines taking were considered in the light not of “compliance” or “adherence“, but of concordance, negotiated between doctor and patient. As a patient with a fairly substantial track record in orthopaedic procedures, I have been repeatedly impressed by the care with which my ideas about treatment, as well as my simple needs, were considered, apart from one particularly memorable infantilising conversation about my catheter.
If there are any bad guys in the story, it is the managers … described … as “corporate rationalists”.
If there are any bad guys in the story, it is the managers, also described, awkwardly, as “corporate rationalists”. The conflicts created by resource constraints are Increasingly well understood in the NHS: Charlotte Williamson describes them as turning doctors into “double agents” – a striking characterisation of potential divided loyalties.
I think some clinicians who read this book will abreact, finding the case over-stated, and believing that we have made enormous strides in the last couple of decades towards genuine shared decision-making and greatly increased patient autonomy. However, the problems keep coming, and Williamson provides a range of examples of sub-optimal care and disregard for patients which still demand attention.
Responses to the COVID-19 pandemic have radically altered the way in which doctors and patients communicate and relate.
This book comes at an important time, when responses to the COVID-19 pandemic have radically altered the way in which doctors and patients communicate and relate. It seems likely that hybrid clinical services, incorporating both face-to-face and digital consultations and surveillance are likely to become a permanent fixture in the NHS, bringing their own problems – and opportunities – about communication, understanding, diagnosis and trust.
Patient input into how these services are best configured, developed and used will be essential, and provides another opportunity to try to create greater equity, autonomy and mutual respect between patients and clinicians.
Featured book
Patients’ Emancipation: Towards Equality. Charlotte Williamson, 2021. Pub: Quacks Books, York, England. £15. ISBN 978–1-912728-36-7
Banner image by Markus Winkler at Unsplash
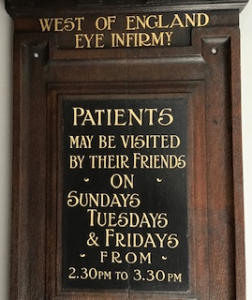
Image in article from Roger Jones