[wp_time_to_read]
Most of the time, GPs in the NHS and family doctors in the US can compare notes about our work, our training, our values and feel like we are two species from the same genus — generalists. Our minor differences came from living in different environments. In my 50 years of being a doctor the structure of medical care in the US and the role of family doctors in communities has gone through organisational changes that have alternately threatened and supported what we do. But so have GPs in the NHS. The appendix to William Faulkner’s arguably most famous book, The Sound and the Fury,° ends with his words about the generations of a black family who have served the dying dynasty of white Southerners: “They endured.” Endurance and perseverance have characterised generalists forever. We endure. In his Nobel Prize speech, Faulkner spoke of his belief that “man will not merely endure but will prevail”. But maybe not family doctors, at least in the US.
Endurance and perseverance have characterised generalists forever. We endure.
While GPs and family doctors remain similar species, we work in radically different funding systems which is more apparent now than any time in history. After a two decade long flirtation with capitated population care in the 1980s Health Maintenance Organizations (HMOs) where primary care worked on a budget that could be adapted to particular populations, US health care reverted back to production models of fee for service care. Volume drove revenues. Despite occasional calls for ‘quality’ based payment that disconnected payment from throughput, the vast majority of physicians are paid through formulae that put a priority on ‘productivity’. Even residency programs in family medicine require certain “numbers of visits” to qualify for certification.
Everything in medicine in the US is designed to generate revenue. What happens, then, when the faucet is suddenly turned off? With the adjustments to COVID-19, our waiting rooms are empty, clinics are being consolidated or closed, family doctors are being redeployed to urgent care, respiratory care or hospital services and hospitals and health systems that thrive on the revenues generated by the volume of referrals are devoid of all but a few patients while the system prepares for the COVID tsunami?
Despite the rapid increase in family doctors employed by hospital or large physician organisations, the majority still practice in small independent single specialty groups. Family doctors still operate on the same principles as local small businesses that rely on customers to support them and, as a result, are subject to the same effects that are crushing restaurants and shops up and down the streets of America.
The view from family medicine on the ground
The extraordinary weekly reports generated by the Larry Green Center° from a national sample of family practices during this pandemic, begins to paint a picture° of how the radical changes driven by the pandemic feel on the ground in communities.
By the end of March, two thirds of family physicians lacked needed personal protection equipment, 70% lacked COVID testing capability and 19% of offices are not doing routine care. All are relying on non-face to face visits. Only 34% of physician practices have enough cash on hand to last four weeks, 60% of offices were uncertain about being able to reopen in four weeks because of staff illnesses and almost 20% are considering permanently closing in the next four weeks. The authors end with the statement “This is a policy emergency that needs immediate attention”. And remember, those data are from three weeks ago.
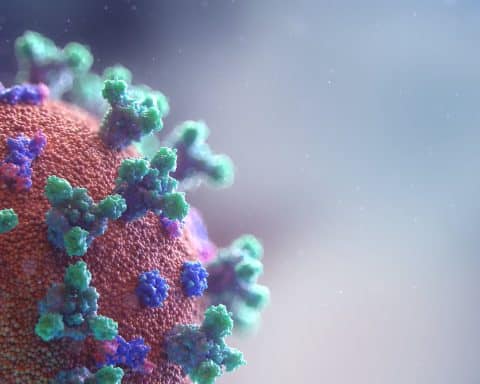
The COVID-19 pandemic has many parallels to the Chixculub extinction event.
There are reliable reports that hospitals are laying off staff and in some cases closing completely. The large health systems are going to furlough or layoff staff at all levels, including physicians. Unemployed or underemployed doctors will become a reality. Primary care is being savaged just when it is most needed to deal with the current demand for management and triage as well as anticipating the future demands of patients who will need preventive and routine care. Tweaking the fee for service system by allowing billing for a telehealth visit isn’t a solution. Shuttered clinics may never reopen, patients will have longer commutes to doctors, and the shrinking revenues and growing unemployment in medical care, which has been one of the most rapidly growing parts of the US economy over the past decade, threatens to undermine economic recovery. Since employer based health care is the norm, front line health workers who are being applauded all across the country will lose their health insurance once they are laid off, becoming uninsured heroes.
The system we work in affects everything
The differences between US general practice and GPs in the NHS could not be more stark. The brilliance of the structure of the NHS was to create a capitated payment system and staff support that assured GPs continuity of income while rewarded access and care. The NHS supports the ability for GPs to adapt to changes, even catastrophic ones, without threatening to bring the entire system down. Once we are beyond the current disruption, even though it will likely go on for years, there will be a primary care system which is GP based in the NHS. Family medicine in the US may be dramatically diminished, if not rendered extinct, if the current payment system that is both poorly and inappropriately funded persists.
The differences between US general practice and GPs in the NHS could not be more stark…. The NHS supports the ability for GPs to adapt to changes, even catastrophic ones…
But without massive universal support for primary care based on capitated, continuous funding for patients, family medicine and other primary care practices are sure to be diminished in number and location in a post pandemic world. Paleontologists are finding fossils that help recreate the timing and location of mammals and deep sea creatures that survived Chixculub. After all, that extinction led to the evolution of mammals and, ultimately, us.
The concept of creative destruction has been used in economics since the early 20th Century and has been applied to everything from proteomics to health policy. But nothing has threatened every aspect of medical care and society with such speed and force as what is happening now. The US in particular has seen over 50 years of uninterrupted economic and physician workforce growth since the passage of Medicare and Medicaid in the 1960s. During this pandemic, destruction in health care is almost assured, but whether it leads to creativity and a renewal in the role of generalists remains a question for the future.
Featured photo by Jimmy Conover on Unsplash