Anmol Arora and Ananya Arora are both medical students at Cambridge.
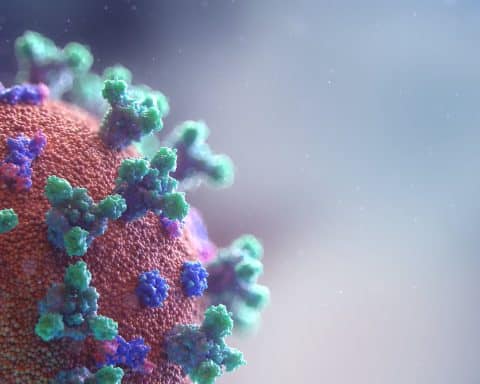
Amongst the extensive disruption exerted by the COVID-19 pandemic on UK healthcare systems, we have already seen years of innovation accelerated within the space of a few weeks. An example of this is the use of video consultations in primary care. Technological advancements are simplifying access to remote video consultations in primary care and will likely remain, in some form, when the COVID-19 pandemic subsides. Whilst the pandemic has also caused disturbance to primary care education for medical students across the country with GP placements being cancelled, it offers potential for long-term benefits.(1)
General practice is an indispensable component of medical school education, offering the opportunity to see a range of patients and practise communication skills. Over the past few years, there have been many calls for an increased focus on primary care in medical school education. Research has found that primary care accounts for a disproportionately low segment of medical school curricula and is underfunded.(2) These problems may be exacerbated if practices substantially change their setups in the coming months to years. There is already a considerable amount of variation in the amount of GP education provided between medical schools across the country and this may grow as access to practices becomes more difficult.(3)
Primary care accounts for a disproportionately low segment of medical school curricula and is underfunded.
In current general practice placements, students are given time to conduct a consultation on their own with the supervising GP reviewing the content and management at the end. By allowing students to access online systems and allowing patients to book onto non-urgent remote consultations with students, GP experience can be simulated virtually with a reduced burden on practices. As they currently do, qualified GPs would review the consultation and perform any indicated follow-up actions, including prescriptions. Unlike current practice, this does not need to be done immediately after the student consultation and they can refer to finished appointment notes.
Healthcare is heading in the direction of telehealth…
Even before the COVID-19 pandemic, there was recognition that changes are needed to increase the availability of primary care placements for students. Virtual experience is not a replacement for physical placements, as students are unable to conduct examinations and would not be exposed to daily non-clinical activities that can only be learned from being there in person. However, given that primary care is moving in the direction of telehealth, it seems reasonable that primary care teaching in medical school should follow to some extent.
References
1. Royal College of General Practitioners. Undergraduate general practice [Internet]. Last accessed: 7th April 2020. Available from: https://www.rcgp.org.uk/training-exams/discover-general-practice/inspiring-future-gps/undergraduate-general-practice.aspx
2. Harding A, Rosenthal J, Al-Seaidy M, Gray DP, McKinley RK, Society for Academic Primary Care (SAPC) Heads of Teaching Group. Provision of medical student teaching in UK general practices: a cross-sectional questionnaire study. Br J Gen Pract. 2015 Jun;65(635):e409-417.
3. Alberti H, Randles HL, Harding A, McKinley RK. Exposure of undergraduates to authentic GP teaching and subsequent entry to GP training: a quantitative study of UK medical schools. Br J Gen Pract. 2017 Apr 1;67(657):e248–52.
4. O’Shea J, Berger R, Samra C, Van Durme D. Telemedicine in education: bridging the gap. Educ Health (Abingdon). 2015 Apr;28(1):64–7.
5. Waseh S, Dicker AP. Telemedicine Training in Undergraduate Medical Education: Mixed-Methods Review. JMIR Med Educ. 2019; 5(1): e12515.