Annabelle Machin is a first 5 GP, Wise GP and WISDOM project intern. She is on Twitter: @drannabellerose
Joanne Reeve is a GP, professor of primary care and leads the WISE GP and WISDOM project.
Emily Lyness is a first 5 GP, Wise GP and WISDOM project intern.
Johanna Reilly is a first 5 GP, Wise GP and WISDOM project intern.
In July 2020, Health Education England published their Future Doctor report, highlighting the characteristics that the doctors of tomorrow will need to master. Examples included generalist skills and the wisdom to make complex judgements, adapt and be a catalyst for change. These all require knowledge work skills.
‘Knowledge work’ is the work that clinicians do to find, create, and use knowledge in everyday clinical practice. Gabbay and May recognised this as the generation of practice-based evidence.1 By observing GPs in practice, they revealed how primary care clinicians rarely access or use research evidence directly, but instead rely on the development of “mindlines”- guidelines-in-the-head. These contain evidence from multiple sources, merged with past experiences and amended through continual learning, to become a clinician’s internal guide to practicing everyday medicine.
Primary care clinicians rarely access or use research evidence directly, but instead rely on the development of “mindlines”- guidelines-in-the-head.
However, the knowledge work of everyday practice is far more complex, requiring us to go beyond managing single or even multiple conditions. Primary2 and secondary care3 clinicians frequently manage indistinct illnesses with no clear pathology, where the patient or their presenting problem may not fit the guidelines. When approaching uncertainty, the temptation can be to keep mining for an underlying cause. However, clinicians have a role as gatekeepers, to minimise exposure to the potential harms of medical intervention.4
As recognised by Health Education England, today’s patients are commonly living with multiple conditions and need tailored understanding and management facilitated by an expert generalist. To enable clinicians to approach complex, indistinct presentations, they require knowledge work skills to facilitate interpretation, explanation and learning. Developing this full range of knowledge work skills has the potential to reduce treatment burden for patients, whilst also decreasing the burden of decision making for clinicians.
….the need for three elements to support clinicians to become better knowledge workers: thinking differently, doing differently and linking differently.
All clinicians in primary and secondary care, use generalist skills in whole person medicine everyday. Strengthening knowledge work skills could foster improved care by expert generalists for future patients. By using these knowledge work skills, tomorrow’s doctors could help to avoid the harms of over-medicalisation of care, promote wider psychosocial and community approaches to supporting people with illness and be the catalyst for positive change required to re-energise our profession.
References
- Gabbay J, May A I. Evidence based guidelines or collectively constructed “mindlines”? Ethnographic study of knowledge management in primary care. BMJ. 2004; 329:1013. doi:10.1136/bmj.329.7473.1013
- Haller H, Cramer H, Lauche R, Dobos G. (2015) Somatoform disorders and medically unexplained symptoms in primary care: a systematic review and meta-analysis of prevalence. Dtsch Arztebl Int 112(16):279–287.
- Nimnuan T, Hotopf M, Wessely S (2001) Medically unexplained symptoms: an epidemiological study in seven specialties. J Psychosom Res 51(1):361–367.
- Heath I. Divided we fail. Clin Med (London) 2011;11(6):576–586.
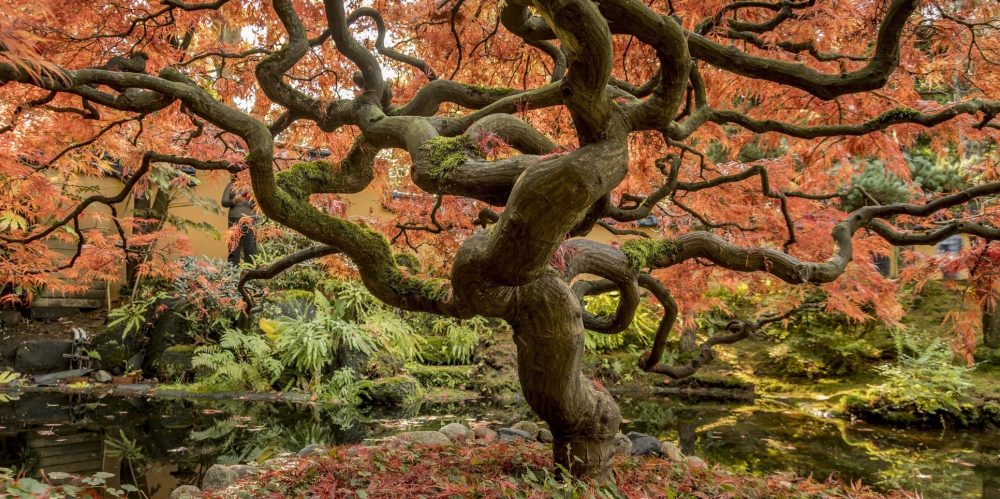
Featured image by Faye Cornish at Unsplash