Marcus Stevens is a GPST1 in Bath, Somerset. He has an interest in global health and recently returned to NHS training following three years working in west Africa.
Marcus Stevens is a GPST1 in Bath, Somerset. He has an interest in global health and recently returned to NHS training following three years working in west Africa.
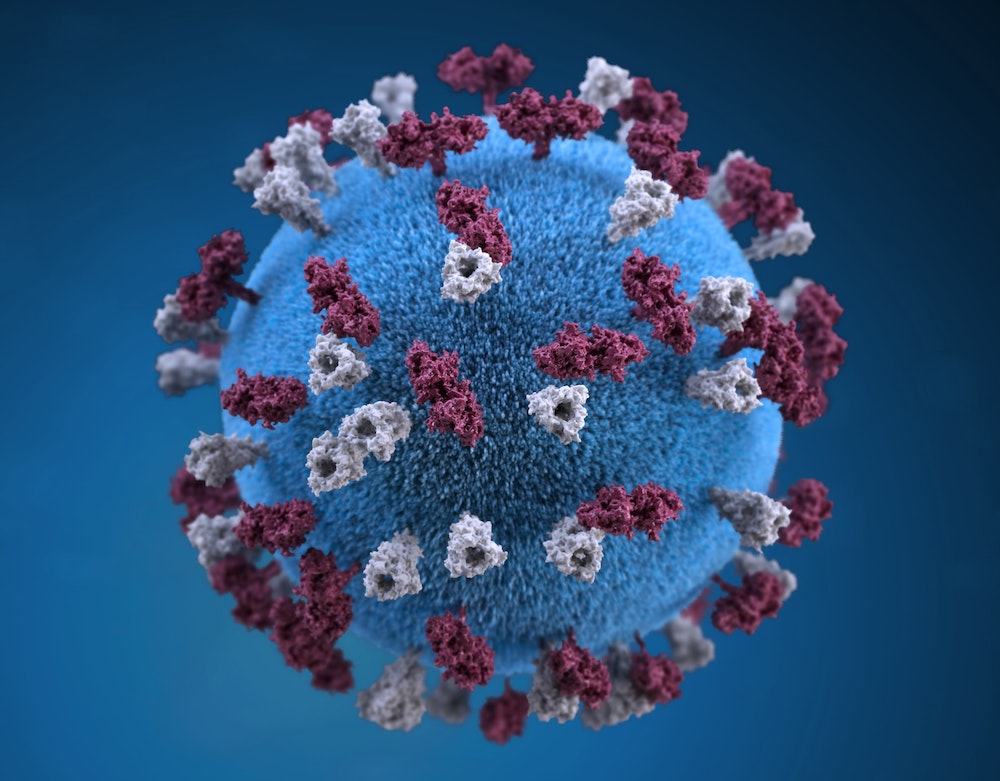
The COVID-19 pandemic is expected to pose an unprecedented challenge to the NHS’ provision of healthcare over the coming months. Epidemiological modelling predicts° a burden of disease at least 8-times greater than current critical care capacity with several European healthcare systems already overwhelmed. Practices across the country, including Somerset’s Frome Medical Practice (FMP), are putting in place preparations needed to provide a breadth of primary care services never before seen.
We aim to avoid pockets of misunderstanding and ensure everyone has access to regular updates drafted by someone who had reviewed up to date medical literature and national guidelines.
These initial briefings evolved into the intra-practice communication model employed for the past two weeks; a morning pre-clinic clinician briefing, lunchtime practice meeting and an evening email update. We aim to avoid pockets of misunderstanding and ensure everyone has access to regular updates drafted by someone who had reviewed up to date medical literature and national guidelines. Whilst many practices will be utilising WhatsApp groups for communication it was felt these posed a risk of overloading staff with information at all hours and so have been avoided.
As the pandemic progresses a significant correlation between age and mortality has been demonstrated, alongside the risk posed by chronic co-morbidities. Wu and McGoogan’s paper° published in late February calculates mortality at 14.8% in those over 80. These data allow one to initiate evidence-based treatment escalation discussions. This has been a priority within frail patient populations in the past weeks and will likely underlie very difficult decisions over the coming months.
There will be deteriorating patients whom are not considered suitable for hospital admission and will need to be managed in their own homes.
Current modelling suggests a prolonged and overwhelming demand on NHS hospital capacity. As a result, there will be deteriorating patients whom are not considered suitable for hospital admission and will need to be managed in their own homes. While these represent the tip of the community iceberg there will be many more unwell or self-isolating who will require support.
This community burden arguably poses the greatest challenge in our national response. It will require the development of extensive multi-disciplinary networks incorporating a wide range of individuals and organisations co-ordinated in order to identify and respond to the changing needs of the population.
In Frome, the foundations of such a network were already in place. Operating since 2013 Health Connections Mendip have built a community ecosystem harnessing the energy of local individuals to provide patients with access to services to ease loneliness, build friendships and pursue activities. A team of Health Connectors act as the bridge between patients and those organisations in the community best placed to help.
It was predicted the following would represent the greatest need in the coming months; food, transport, medication and social contact. A process of community mapping is currently establishing the groups, restaurants, shops, food banks and individuals who are committed to supporting the community and how they are best placed to do so.
Education will form the next stage of preparations, ensuring all those who may encounter people struggling know where to signpost them and how to assist them in accessing support. We hope this approach, a network of the community for the community, will be capable of addressing the predicted burden of community need in the coming weeks.