Academic positions offer novel ventures and variation for practicing GPs, but both roles can pull you in opposite directions. Instead, use them to complement each other, and don’t rip at the seams…
Medical degrees offer value that extends beyond clinical practice. The multifaceted modern medical curriculum aims to create versatile graduates, developing scientists, leaders and teachers too.1, 2 It is from this platform that GPs can springboard into many other complementary spheres – revitalising a CV, and repairing frazzled mindsets.
I have both science and medical degrees, and teach life sciences and professional development skills across university programmes, as well as practicing clinically as a locum GP. A dual career has been intellectually stimulating, and without a doubt worthwhile, but not without its challenges. Seven years on from my start-point, I’ve realised how this road can be made more easily accessible, and the journey along it less potholed. GP colleagues; if striving to build a portfolio career, be reassured that balancing clinical practice and academia is entirely achievable, allowing you to remain comfortably “in” both realms.
Realise the wealth of experience you already have
Entry into academia is often seen as more difficult than the reality. Many applicants may feel they won’t fit the job description; fearing lack of experience, teaching qualifications, or other degrees such as an intercalated or pre-med BSc, or indeed a PhD.3 Look beyond this, and recognise that your background is already relevant. Some of this is tacit – disguised, understated – but is there nonetheless, and can be easily uncovered.
Make use, therefore, of all the acumen that you’ve worked so hard to earn, and don’t rule yourself out.
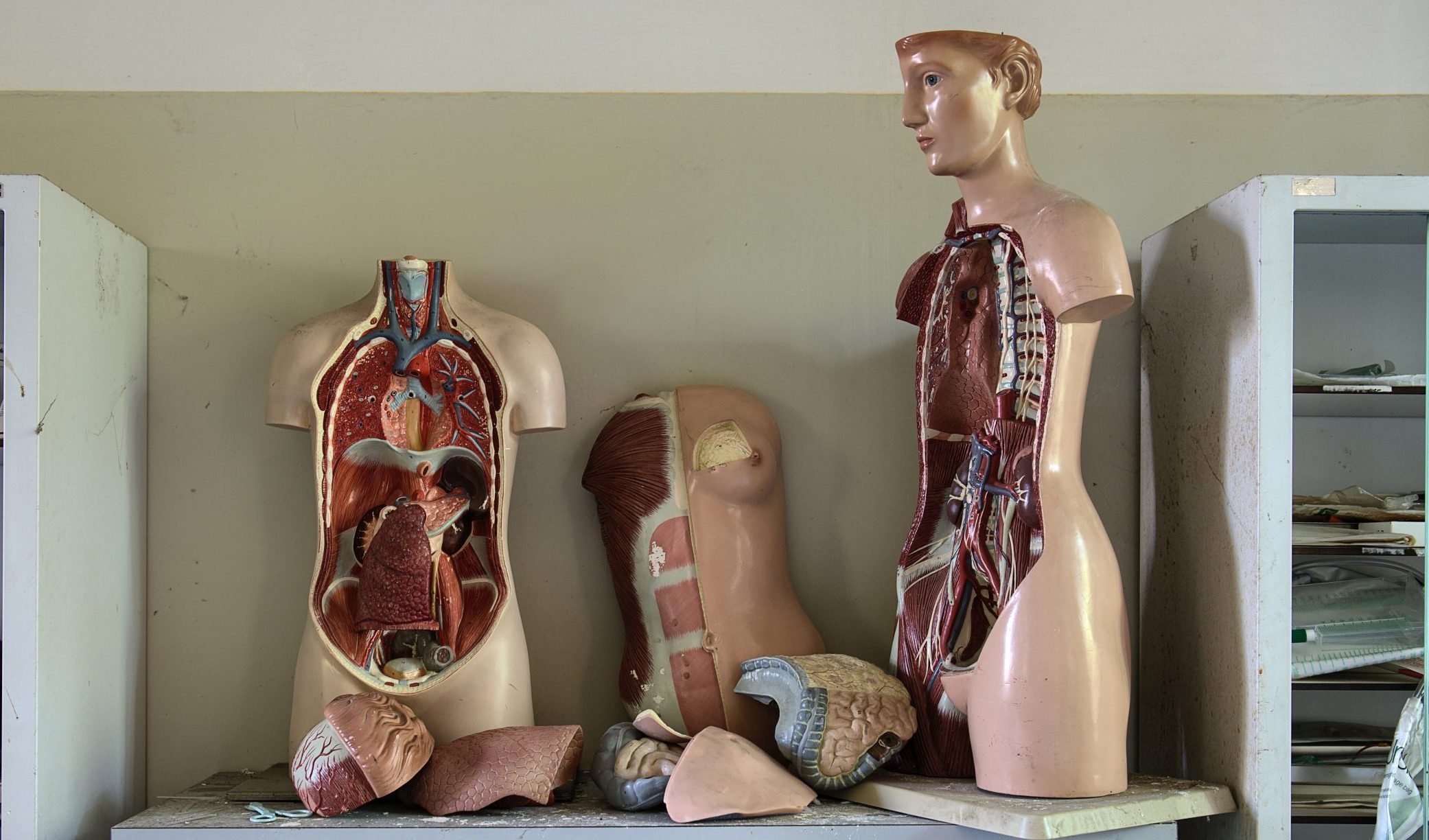
Take first, what you’ve learned at university, and observed in practice. You’ve an arsenal of clinical experiences and narratives to share with students, and have covered a broad foundation of basic sciences; anatomy, physiology, pharmacology, and more. You’re also proficient in consultation skills, and dependent on your background and stage of training, may also have specialist knowledge to impart. All these capabilities align with many different stages of the curriculum.
Look next to the teaching you’ve been responsible for; remember, opportunities exist beyond the scope of tradition. Reflect upon all formal and ad hoc experiences; bedside teaching, grand round presentations, outreach, supervision of shadowing medical students, and sessions with peers.4 Never forget the educational contact you share with patients. GPs are already everyday teachers; giving explanations of diagnoses and treatments, providing lifestyle advice, problem solving, and answering queries.
On advice from regulatory bodies, universities now consider and recognise a wider range of essential qualities than just teaching experiences alone when recruiting; key competencies, aptitude and leadership skills to name a few. Make use, therefore, of all the acumen that you’ve worked so hard to earn, and don’t rule yourself out.
Learn from new experiences, and be opportunistic
Moving into an academic role emphasises the chance to further your own learning – not just from colleagues, but also from your students, who act as an important benchmark for quality assurance in education. The concept of “teach the teachers” cannot be overstated – all educators, regardless of age and experience, can continue to develop their teaching abilities5. The transition from a didactic to a facilitative academic was my own significant turning point, empowering students to be self-directed, independent scholars.
Whether clinicians can equally be branded “scientists” is debatable, and the science content of some curricula is becoming increasingly restricted.6 Nonetheless, basic science remains a cornerstone of medical practice, and there are many opportunities available in teaching the core sciences. Equally, skills relating to the scientific method – critical appraisal of literature, formulating hypotheses, data handling and interpretation – are the skills that feed forward into clinical practice – into evidence-based medicine and service improvement. And making you, and your students, more informed doctors.
Choose a post carefully, and the timing in relation to your clinical training. Multiple access points are possible, each with their relative benefits, and limitations. Enquire about opportunities and scholarship time available to further yourself along the way – leadership, academic writing and other short courses are some examples, alongside funding for higher degrees.
Always look to the future
Decision making is equally complex; so, acknowledge the push-pull factors. What do you enjoy most? What is forward facing? What pays the bills?!E
arly in my journey, when a suitable permanent post hadn’t yet opened and there was a definite period of uncertainty, a senior colleague suggested I sit back and consider the answer to a very valid question carefully; if an academic position could be served up on a silver platter, what would it be?
Doing so proved a valuable exercise, in projecting where I’d like to be standing in a year’s-time. And then, in two, five, and ten-years from that point. It helped establish a timeline, making me realise the hurdles on the track that needed to be cleared, and the commitments I had to fulfil. Both roles require a certain amount of hoop-jumping, for which foresight is a guiding beacon. Progression to senior academic roles might require further qualifications – certainly leadership and administrative experiences, and writing for publication, are important checklist points. Of course, continuing commitment to an appraisal process is expected from a GP – a number of clinical shifts each year, alongside professional development, and reflections on practice, in tandem with academic growth.
Be aware of the balancing act between your two identities, and the questions you may ask yourself.7 Am I prioritising one over the other? Should I be giving one of them up? Decision making is equally complex; so, acknowledge the push-pull factors. What do you enjoy most? What is forward facing? What pays the bills?!
Most importantly, recognise what you want to teach, and ask for it. Your individual expertise always has weight and value, and don’t be afraid to request a change if you feel it is needed to refresh your routine.
Outcome
The culmination of this iterative route, though marked with episodes of uncertainty, has been the development of a synergistic portfolio career, offering welcome daily variation, and infinite reward.8 The implications are much wider, however. It is the duty of doctors to realise their teaching potential, and their commitment to pass on their wisdom. The next generation of doctors will only be as good and knowledgeable as those who precede them. What better way for them, and for you, than realising the teacher you already are?
References
- Jefferies R, Sheriff IH, Matthews JH, Jagger O, Curtis S, Lees P, Spurgeon PC, Fountain DM, Oldman A, Habib A, Saied A, Court J, Giannoudi M, Sayma M, Ward N, Cork N, Olatokun O, Devine O, O’Connell P, Carr P, Kotronias RA, Gardiner R, Buckle RT, Thomson RJ, Williams S, Nicholson SJ, Goga U. Leadership and management in UK medical school curricula. J Health Organ Manag. 2016 Oct 10;30(7):1081-1104.
- Ratte A, Drees S, Schmidt-Ott T. The importance of scientific competencies in German medical curricula – the student perspective. BMC Med Educ. 2018 Jun 19;18(1):146.
- Lamb EI, Alberti H, McKechnie DGJ, Park S, Pope L, Thampy H. Developing a career as a GP educationalist: contemporary challenges and workforce solutions. Educ Prim Care. 2023 May;34(3):113-118.
- Alberti H, Rosenthal J, Kirtchuk L, Thampy H, Harrison M. Near peer teaching in general practice: option or expectation? Educ Prim Care. 2019 Nov;30(6):342-346.
- Allsop S, McKinley RK, Douglass C, Pope L, Macdougall C. Every doctor an educator? Med Teach. 2023 Jun;45(6):559-564.
- Utz PJ, Jain MK, Cheung VG, Kobilka BK, Lefkowitz R, Yamada T, Dzau VJ. Translating science to medicine: The case for physician-scientists. Sci Transl Med. 2022 Feb 16;14(632)
- McElhinney Z, Kennedy C. By accident or design? An exploration of the career pathways, experiences and identities of academic GPs using composite narratives. Educ Prim Care. 2021 Sep;32(5):266-271.
- Baumgardt D. From anatomy to GP and back again: lessons from an academic full-circle.