Richard Armitage is a GP and Honorary Assistant Professor at the University of Nottingham’s Academic Unit of Population and Lifespan Sciences. He is on twitter: @drricharmitage
Richard Armitage is a GP and Honorary Assistant Professor at the University of Nottingham’s Academic Unit of Population and Lifespan Sciences. He is on twitter: @drricharmitage
NHS Digital provides monthly statistics regarding appointments in general practice in England.1 While there is substantial variation in the total number of appointments each month, trend line analysis reveals that the total number of monthly appointments has increased by 30.9% between December 2017 (approximately 22 million) and October 2023 (approximately 28.8 million). Additional clinical roles, such as advanced nurse practitioners and physician associates, have been introduced and expanded in general practice during this time. This explains some, but not all, of the increased delivery of patient care.
These NHS Digital statistics are also presented by type of professional (for example, GP or nurse). Trend line analysis reveals that the total number of monthly appointments conducted by GPs increased by 11.7% between December 2017 (approximately 12 million) and October 2023 (approximately 13.4 million).1
NHS Digital also provides statistics on the general practice workforce in England (provided quarterly prior to, and monthly since, July 2021).2 Trend line analysis reveals that the total number of full-time equivalent (FTE) fully-qualified (excluding those in training) GPs decreased by 5.4% between December 2017 (approximately 28 750) and October 2023 (approximately 27 200). Accordingly, the average number of monthly appointments conducted by each FTE GP in England increased by 18.2% from December 2017 (approximately 417) and October 2023 (approximately 493) (Figure 1).
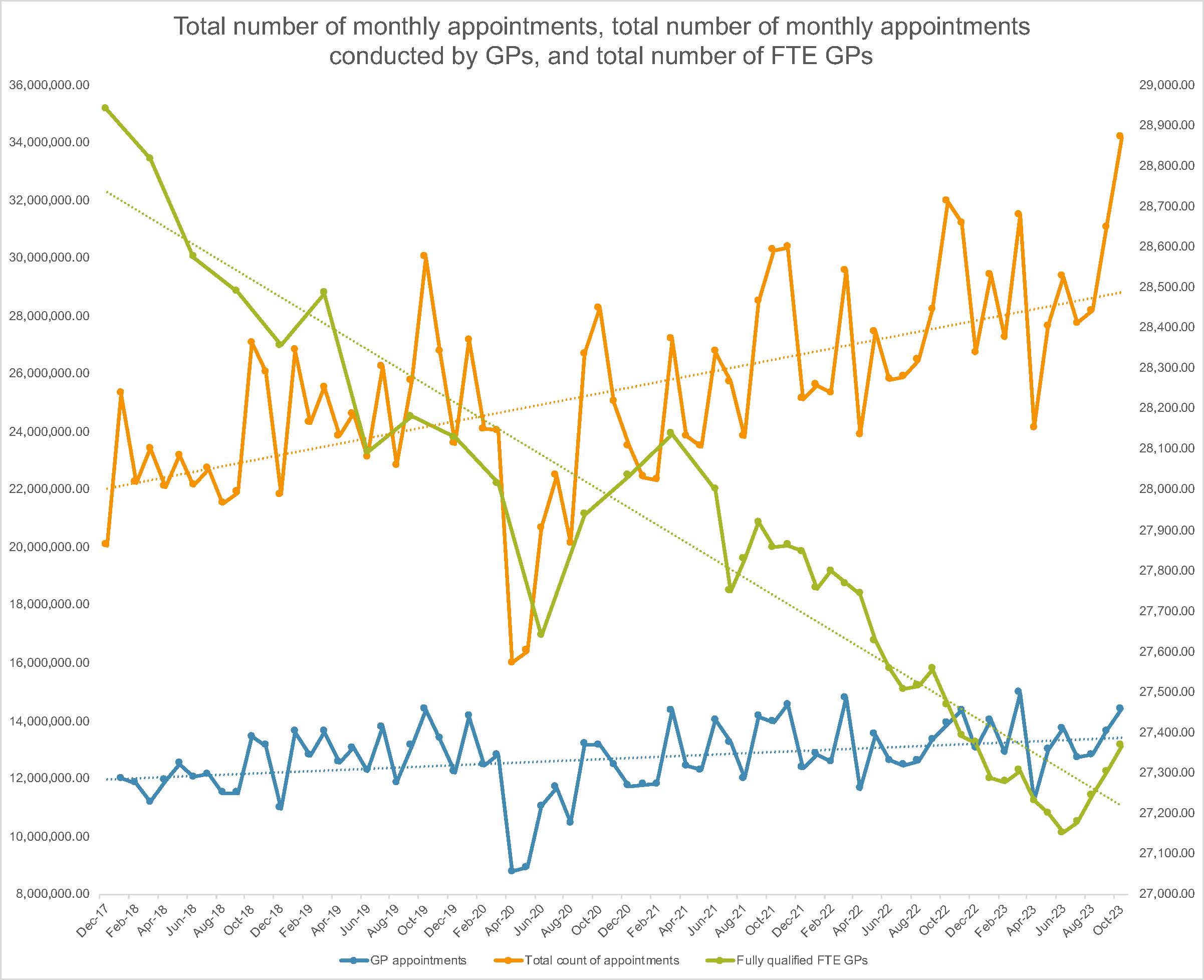
Simultaneously, the nature of the care provided in general practice has and continues to become increasingly complex, due to a constellation of problems including ageing populations, multimorbidity, polypharmacy, antimicrobial resistance, and language barriers. Accordingly, each FTE GP in late 2023 is caring for a substantially greater number of patients who are considerably more complex than only 6 years previously. This poses obvious threats to both the quality and safety of that care.
To deliver these additional appointments, the proportion of consultations that take place remotely (telephone or video modality) has substantially increased (this was triggered by the first COVID-19 national lockdown, and remains markedly above its pre-pandemic baseline).1 However, while remote consultations can facilitate increased patient convenience and general practice productivity, they are associated with threats to patient safety.3
GPs in England are working under profound and rapidly increasing pressure. These conditions are associated with higher levels of burnout (which drive GPs to quit, thereby compounding the problem),4 which in turn are associated with patient safety risks.5 Mitigation is therefore urgently required, including improved usage of other primary care roles (for example, community pharmacists), empowering self-management, and enhanced prevention.
References
1. NHS Digital. Appointments in general practice. 2023. https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice (accessed 12 Dec 2023).
2. NHS Digital. General practice workforce. 2023. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services (accessed 12 Dec 2023).
3. Payne R, Clarke A, Swann N, et al. Patient safety in remote primary care encounters: multimethod qualitative study combining Safety I and Safety II analysis. BMJ Qual Saf 2023; DOI: 10.1136/bmjqs-2023-016674.
4. Sharrock K. Burnout is forcing more and more GPs to quit the NHS. The Guardian 2023; 6 Apr: https://www.theguardian.com/society/2023/apr/06/burnout-is-forcing-more-and-more-gps-to-quit-the-nhs (accessed 12 Dec 2023).
5. Hall LH, Johnson J, Watt I, O’Connor B. Association of GP wellbeing and burnout with patient safety in UK primary care: a cross-sectional survey. Br J Gen Pract 2019; DOI: https://doi.org/10.3399/bjgp19X702713.