John J. Frey III is an emeritus professor of Family Medicine and Community Health at the University of Wisconsin School of Medicine and Public Health. He is on Twitter: @jjfrey3MD
John J. Frey III is an emeritus professor of Family Medicine and Community Health at the University of Wisconsin School of Medicine and Public Health. He is on Twitter: @jjfrey3MD
Competition, not collaboration, has always characterized medicine in the US.
Until the 1970’s, US GP’s were most often single handed or in small groups out in communities competing for patients. But today, with corporate health controlling most of the care, every average size town has a 50,000 square foot building full of machines and specialists that would ordinarily be called “hospitals”, and where GP’s groups may occupy an office on the third floor decorated in company colors. So, instead of the minor skirmishes with minimal casualties that small town docs used to have, health care in the US is now a series of epic battles, advised by investment bankers, often ending with loss of services where people need them most, physicians’ lives being disrupted, and facilities, mostly in small towns and rural areas, being closed. That is what is called “competition” today.
In mid-20th Century, GPs could convince legislators, most of whom had a family doctor, to support funding for education and primary care. But now, legislators, like most Americans, get care from a panoply of specialists and, consequently, the power now lies in hospitals, Pharma, sexy research that promises big breakthroughs, and lots of talk about cures rather than a need for personal care. The vast majority of COVID-19 relief funds went large cities and big hospital systems. Mayo Clinic, for example, with a multibillion dollar endowment, received $338 million and returned half of it. Yet the entire state of Wisconsin got $56 million. Hospitals in New York State got 12% of the total relief funds but have only 6% of the population of the US. Wisconsin, with 1.75% of the US population got .05% of the relief funds.
Health care in the US is now a series of epic battles …. often ending with loss of services where people need them most.
When vaccines became available, a rational approach to distribution of supplies would have been to create a dual effort with large vaccine centers that were maximally efficient and also get the vaccine to family doctors, pediatricians and general internists located in communities who served the more difficult to reach patients. Instead of being at the forefront of the vaccine campaign as they had been with almost every vaccine in history, US primary care physicians were enlisted when the campaign seemed to be floundering and the large vaccination centers were being closed. The administration knew that personal physicians were trusted more than government, particularly with the doubters among the vaccine hesitant, but despite that, seemed to believe that mobilizing the National Guard to staff drive through vaccine centers was more effective. But it isn’t for those who need the vaccine the most and resist it the hardest, so we are having yet another wave that threatens the country.
General Practice in the UK has had, and continues to have, many issues which need remedying to create an effective and satisfying role in the NHS. But GPs can have a powerful voice. If primary care truly is a common good, as the recent US report states, it needs a unified common voice to counter the very loud voices of hospitals and medical schools.
If primary care truly is a common good, as the recent US report states, it needs a unified common voice to counter the very loud voices of hospitals and medical schools.
Working together also means training together and teaching together and doing away with the Balkanization of primary care. Now may be the time when generalists drop past excuses for maintaining parallel residency programs and form large and effective joint training for community based physicians who then go on to practice jointly.
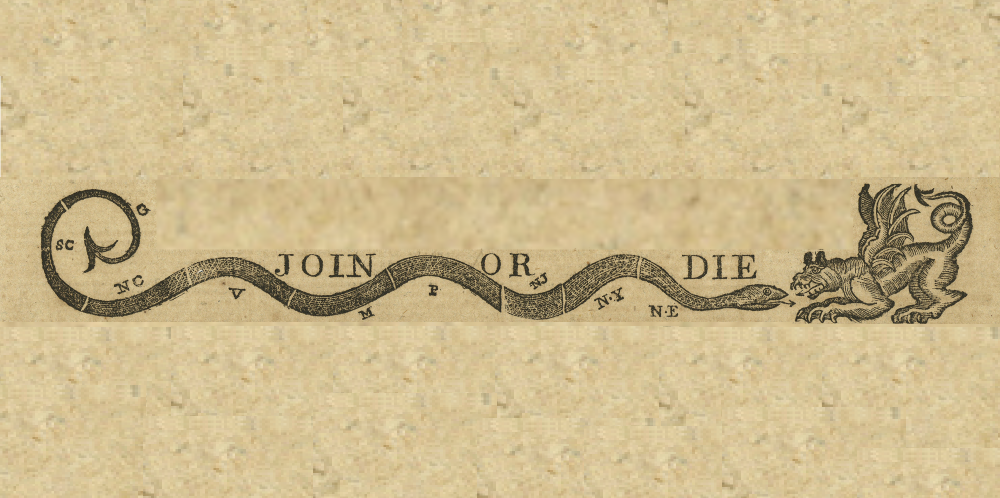
Generalists should recreate the pre-Revolutionary War flag that depicted a snake cut into pieces representing different colonies and the words “Join or Die” underneath it. True then. And, as far as primary care in the US is concerned, true now.
References
1. Gouda D, Singh PM, Gouda P, Goudra B. An Overview of Health Care Worker Reported Deaths During the COVID-19 Pandemic. Journal of the American Board of Family Medicine : JABFM. 2021;34(Suppl):S244-s246.
2. Epperly T, Bechtel C, Sweeney R, et al. The Shared Principles of Primary Care: A Multistakeholder Initiative to Find a Common Voice. Family medicine. 2019;51(2):179-184.
3. McCauley L PR, Meisenere M, Robinson S.K (eds). Implementing High-Qualtiy Primary Care: Rebuilding the foundation of Health Care. In: Medicine, ed. Washington, DC: National Academies Press; 2021.
Featured image is Paul Revere’s version of the Join or Die cartoon seen on the Massachusetts Spy, on Wikimedia Commons