Another busy surgery in another overfilled and stressful working week. A routine appointment for a medication review. A brief check of the notes and it is a patient you don’t know, taking eight different medications for four separate problems. They’ve been recalled by our trusted IT systems to see a GP because QOF mandates it. You’ve probably got 10 minutes, 15 if you are fortunate. Where do you even begin to try and spend that time working with that individual patient on their overall care plan?
You’ve probably got 10 minutes, 15 if you are fortunate. Where do you even begin to try and spend that time working with that individual patient on their overall care plan?
Polypharmacy is an increasingly common patient problem we see in primary care. 15%of NHS patients in England take five or more medications on a regular basis, a whopping 8.4 million people. This number only tells part of the story as older adults, ethnic minorities, patients with mental health diagnoses and those from areas of social deprivation are over represented.1 As patients live longer they collect diagnoses like a game of multimorbidity monopoly. Another trip around the board, another two cards for your collection. Well- intentioned generalists and specialists then try to help manage how these conditions are affecting people’s lives, or reduce the risk of significant future health events. This often results in prescribing medications that are supported by evidence-based guidelines. But how often do these guidelines acknowledge or complement each other? How drastically has the fragmentation arising from clinical sub-specialism driven holistic medicine out of so many consultations?
Nobody wants or benefits from the current status quo when it comes to managing polypharmacy. Patients can feel fed up with taking or monitoring their medication. Side effects cause significant harm with 10% of hospital admissions being due to adverse drug interactions.2 That number doesn’t capture the people affected that didn’t warrant admission. Clinicians are aware of the problems with polypharmacy and want to change it but describe feeling unable to act. Maybe due to lack of time, other workload pressures, or working in a system that doesn’t support the work needed to comprehensively review patient’s medications with them. For some it is fear. Fear of harming someone by stopping or reducing a medication: ‘If I don’t follow this guideline and something happens it’s the GMC for me.’ ‘Oh, well that medication was started by a specialist so I can’t stop that, they know more than me.’
Clinicians are aware of the problems with polypharmacy and want to change it but describe feeling unable to act.
The recently published NIHR funded TAILOR report3 was commissioned to try and break down those barriers to deprescribing. An extensive and comprehensive synthesis of published data relating to deprescribing for older adults to see not only what is known about deprescribing but how can we best try and do it in practice. And it’s good news – deprescribing is safe, effective and acceptable for clinicians. Importantly there is no single best approach to how we do this. We can personalise it to our local needs. What we need to consider within our local practices, PCN, CCG, ICB, is how do we change our current practice to better support this work? Deprescribing is not a silver bullet, but it is an important part of how we change our approach to managing this problem. Integrating this important clinical skill into our daily practice needs to be prioritised. TAILOR goes on to suggest a framework for how we can work together across an extended MDT to improve medicines management and reduce the burden of illness patients often feel as a result of their medication regime.
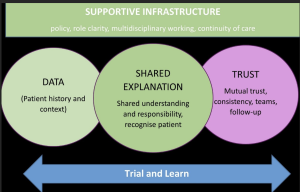
IMAGE: The DExTruS framework for managing polypharmacy. Reproduced from Turk et al4
This framework, shortened to DExTruS, stands for Data, Explanation, Trust, and Supportive infrastructure. We need to consider what data we need, how we collect it and from what sources. How we use that data to make shared decisions with our patients, and importantly how we build trust into that relationship while recognising the challenges of providing continuity to our patients in the current workforce climate. Also recognising this is a longitudinal process that should be built into all consultations, not a single annual event. While this may not come as a surprise research shows that we sometimes lack both the skills to do this and the confidence to use them.5 As expert generalists and within our wider MDTs we have the capability to do this work. What needs to change is the infrastructure to support how we do it and create the capacity for it. The task lies in how we change our ways of working to incorporate it. We now know it is a safe, effective and acceptable intervention for us to implement. The greatest challenge and therefore the biggest opportunity here is in making it happen
REFERENCES
- Department of Health and Social Care. Good for you, good for us, good for everybody. A plan to reduce overprescribing to make patient care better and safer, support the NHS, and reduce carbon emissions. 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1019475/good-for-you-good-for-us-good-for-everybody.pdf (accessed 22 Feb 2023)
- Swinglehurst D, Fudge N. The polypharmacy challenge: time for a new script? Br J Gen Pract 2017; DOI: https://doi.org/10.3399/bjgp17X692189.
- Reeve J, Maden M, Hill R, et al. Deprescribing medicines in older people living with multimorbidity and polypharmacy: the TAILOR evidence synthesis. Health Technol Assess 2022; 26(32): 1 –148
- Turk A, Wong G, Mahtani KR, et al. Optimising a person-centred approach to stopping medicines in older people with multimorbidity and polypharmacy using the DExTruS framework: a realist review. BMC Med 2022; 20(1):297.
- Reeve J, Britten N, Byng R, et al. Identifying enablers and barriers to individually tailored prescribing: a survey of healthcare professionals in the UK. BMC Fam Pract 2018;19(1): 17.
Featured photo by Ksenia Yakovleva on Unsplash