The Eisenhower matrix is an eponymous task management tool attributed to the late US President which helps to organise and prioritise tasks by urgency and importance, so you can focus on getting the most urgent and important things done first. So, am
Peter McNelly provides an introduction to the role of the mental health practitioner in general practice, and how they can help reduce the workload of GPs.
John Spicer and Carwyn Hooper unpack the Hippocratic duty to teach for 21st century primary care.
It is important that GPs are able to recognise this phenomenon, and to not dismiss the SMI lifestyle as a harmless pursuit for frivolous Gen-Z-ers. Richard Armitage unpacks the health implications.
Some patients with medically unexplained symptoms (MUS) suffer years of referrals and inconclusive tests. Others find themselves overlooked by health care services and feel forgotten. However, diagnostic delay may be due to a disease being rare. Stephen Walker and colleagues offer a
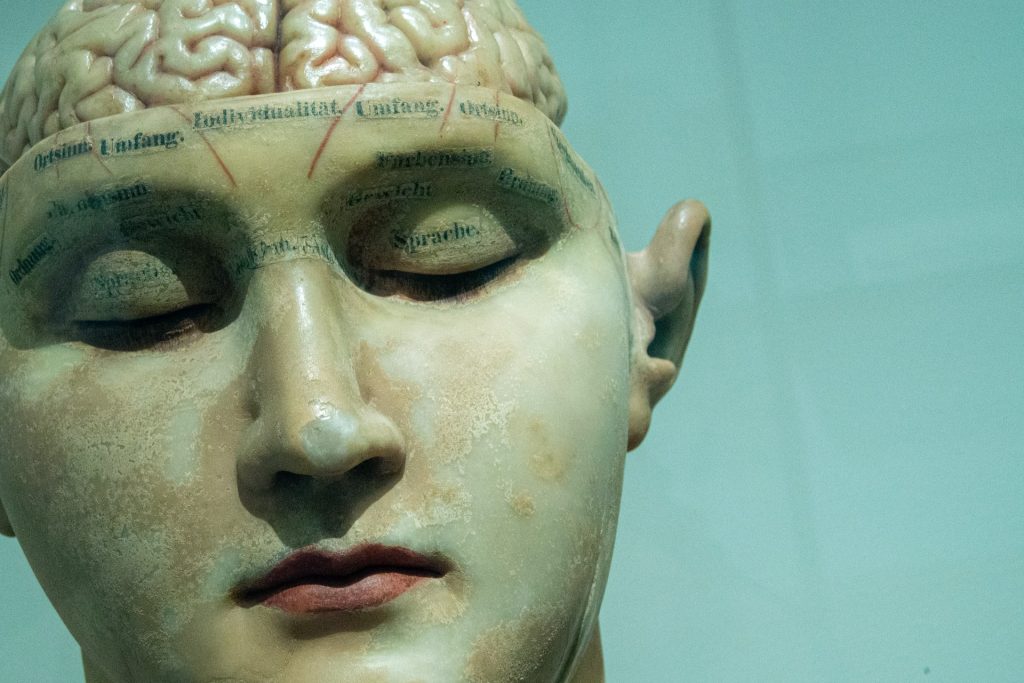
New research into the serotonin theory of depression raises two separate, but related issues. The first is our understanding about the aetiology of depression. The second is understanding why we prescribe antidepressants. Nada Khan reflects on what this means for general practice.
Lisa Broom, Frances Dutton (GPs), and Chris Bird (Paediatric A&E Consultant) reflect on a fellowship that allowed both GPs to have one foot in Birmingham Children's Hospital's busy emergency department and the other in primary care in the city, with time to
Richard Armitage examines the 'Deborah James effect' on cancer awareness. How should we enhance the benefits and mitigate any harms of publicly shared celebrity cancer stories?
People living in more affluent parts of the world with better healthcare and less disease tend to have a lower view of their health than people in poorer areas, where disease is more prevalent and healthcare less well-developed. Ben Hoban asks what
Rebecca te Water Naudé and Peter Young suggest that GPs may have duty to discuss the pros and cons of patients who contemplate crowdfunding for cancer treatment, and outline some of the issues.
Richard Armitage looks at the health needs of people who work away from home, be they itinerant telecommuters or contract-workers in haulage and construction - should general practice be evolving to meet the access needs of this group? Join the discussion!
One of medicine’s great strengths is the precise use of language it employs to describe what and where it is diagnosing the issue in hand. This, of course, would be fine if we only spoke amongst ourselves in a professional capacity.
Pamela Martin shares the Doctors for Unite vision for the future of primary healthcare in the UK - a call to action!
How and why do we define something as a public health problem? Richard Armitage reflects on the complexities.
There are three levels of general practice: generalist practice approach, general generalist practice and expert generalist practice. Koki Kato explains how they can help GPs explain what they do.
Bakula Patel asks is cracking work-life balance is as simple as considering life-work balance? Comments welcome!
Around 80% of all care in the UK is self-care, but despite people's willingness to initially self-treat, minor ailments contribute to 57 million GP consultations a year. How then can GPs promote continued self-care to patients?
Nada Khan examines the increasing waiting times for ambulances, finding a system under pressure and dilemmas for clinical staff.
Tim Senior reflects on what makes a 'virtuoso' GP. Is a question of detective skills or the ability to establish a rapport?
Richard Armitage argues that good management of hay fever represents an opportunity for general practice to reduce suffering and restore both wellbeing and economic activity to the nation!
At the beginning of my foundation training I had very limited awareness of the diversity of the clinical workforce and was only familiar with 'traditional' doctor roles. However, I was surprised to find myself in the midst of a large, multiskilled dynamic
Approximately 1%–2% of the adult population experience stammering, which can have a significant impact on a person's quality of life. Here, members of the NHS Stammering Network (for staff) describe how best to optimise consultations with this patient group.
In 2020, Sir Michael Marmot and his team at the Institute of Health Equity published ‘Build Back Fairer’ to examine how the Covid pandemic affected health inequalities in England. Nada Khan discuss a grim but inspiring document.
The Department for Work and Pensions has recently announced legislative change that will allow a wider range of healthcare professionals to authorise fit notes. Is this an opportunity for general practice to improve patient access to occupational health support?
Healthcare professionals deploying to and practicing in conflicts and catastrophes can experience a plethora of negative emotions due to perceived or actual transgressions of their core ethical principles. In his final Ukraine report, Richard Armitage gives a powerful personal reflection.
The NHS is facing a backlog that will take years to clear and GPs are likely to be the main point of contact for patients who are suffering as a result. Nada Khan examines the issues.
Richard Armitage investigates the impact of the war in Ukraine on the country’s health worker density.
How can we encourage the development of kindness toward ourselves and others? Is it something we can train, and should it perhaps be a part of the GP curriculum? Touching on their own personal experience of being on the receiving end of
Bhupinder Goraya muses on the concepts of order and randomness in relation to health and primary healthcare. We’ve worked 'bloody hard' to make a random mechanical universe work, in doing so we have ordered our leisure.
Anaemia is a serious public health concern globally, yet WHO's cut-off values for Hgb were established in 1968 using predominantly White populations in Europe and North America. Is it time to update to population specific cut-offs?
How do we support each other when a colleague dies by suicide? A reflection by Louise Stone.
Laura Heath discusses ‘trade-offs’ that we should reflect on in modern primary care. Are we clinical providers or clinical supervisors? Data sharers or data stewards? Secondary care helpers, or expert generalists? If our voice is not heard the ‘trade off’ will be
Nada Khan explores the roles of and our perceptions about primary care multidiciplinary teams, in light of the recent BBC Panorama investigation
General practices and staff have been facing violent behaviour or aggression from members of the public -a global phenomenon now an UK issue. Vasumathy Sivarajasingam asks, what's happening, so what, and what now?
'One man in his time plays many parts' — What is the role of the older, experienced GP? In retiring, this ‘premature abdication’ represents an enormous loss to the NHS. Here, Maxwell Cooper and colleagues outline a vision for a future general
Recent media coverage has focussed on whether patients should be fined for missing appointments. Would a £10 fine change patient behaviour and put an end to this story once and for all? Nada Khan investigates!
The Cynefin framework is believed to encourage the perception of existing structures with new eyes, aiding decision making and simplifying complex concepts. Can this framework help to make sense of challenging GP consultations that may leave GPs feeling inadequate or ineffective?
General public concern over the adequate control of blood pressure is notably high within Ukraine, possibly due to the concerning prevalence of hypertensive disease, public awareness of its associated risk factors, and successful health promotion by primary care and public health professionals.
As we’ve emerged from various lockdowns, large parts of the media have intensified a negative rhetoric against GPs. Annabelle Machin argues that there is still a powerful hope from... talking to each other!
Capacity for undergraduate GP placements is a serious challenge and one that is predicted to become harder in the near future. Here, Simon Thornton, part of the national working group set up to investigate the issue of teaching capacity in general practice