Biological causality for T4 monotherapy not working for some is now established. We can’t now attribute the 10%–15% of people with hypothyroidism not feeling better on T4 as wimps, laggards, or requiring psychological attention. Sarah Cathcart Evans reflects from personal experience of
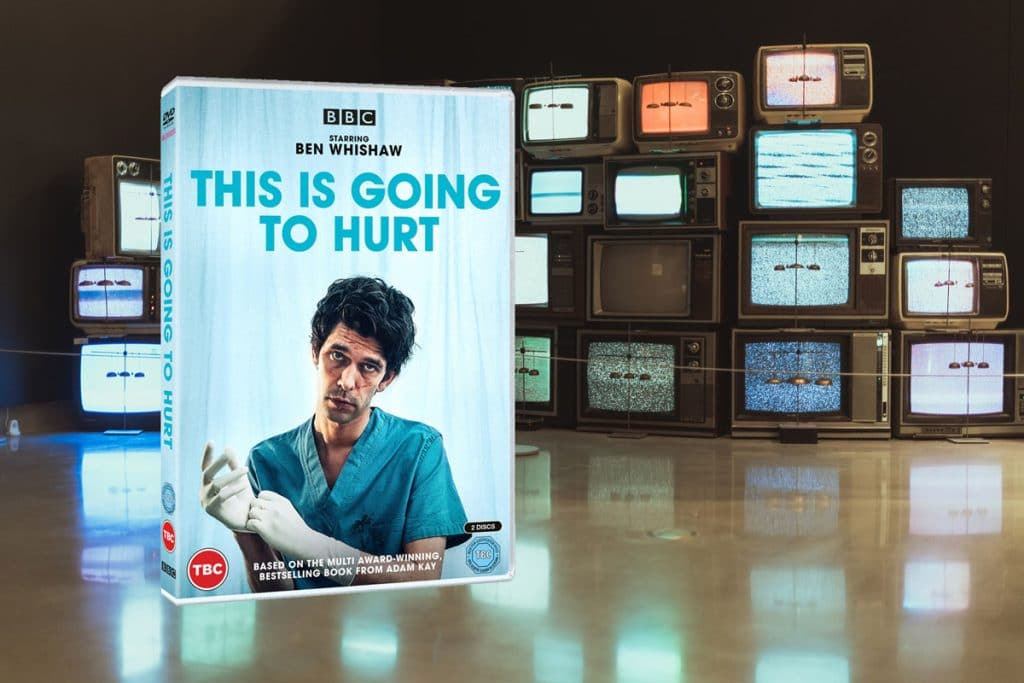
Yathu Maheswaran reflects on what TV 'This is going to hurt' might teach medical trainees
Vasumathy Sivarajasingam argues that improving healthcare for healthcare workers might improve the overall healthcare service as well as the welfare and morale of those who work for it
Drs Laura Heath and Sheena Sharma present their bereavement toolkit, designed to aid healthcare practitioners navigate this potentially difficult space by providing real-world consultation ‘tools’.
Rabia Aftab suggests that the option of ‘doing nothing’ should be shared with patients, but is this nothing actually quite a powerful something?
Samar Razaq reflects on expectations of treatment when an illness is not well understood and medical evidence is lacking or unclear
Giles Dawnay considers practitioner, patient, culture and politics in his reflections on the present and relationship between GP and patient
"Through partnership rather than paternalism, the future patient–GP relationship will embrace the change of the world yet to come." — Nathaniel Roocroft, winner of this year's Kieran Sweeney Prize, sets out a future vision of general practice.
Narinder Bansal and colleagues argue that clinicians should be sensitive to how experiences of poor listening and relating can replicate and trigger wider experiences of marginalisation.
Arthur Kaufman reflects on the good old days for medical writers
Stoic philosophy was based on the recognition that we cannot escape what is destined for us. An acceptance of inevitability has a number of implications for working as a GP. Austin O'Carroll wrestles with fate.
Richard Armitage argues that insufficient sleep should be regarded as a serious problem requiring the urgent attention of public health and primary care practitioners.
Ed Warren asks if the north of England needs its own consultation model. Or will 'levelling up' be sufficient?
It is only in recent years that the physical and emotional burden faced by those in the medical profession has been raised. What can be done at both a structural and individual level to aid the wellbeing of medical staff? Dr Feryad
Joel Brown examines the sales pitch for a career in private general practice, and is left feeling proud of working for the NHS
John Launer reflects that Pather Panchali is a masterpiece in its own right but there are particular reasons why GPs might want to find time to watch it. Few other movies show such a profound understanding of family life among people living
Peter Toon reflects on registering overseas vaccinations in the UK and asks if there are lessons for the NHS as a whole
Kath Brown argues that although Covid has exposed our long-standing domestic drivers of poor health, we simply cannot ignore global health inequalities during a global pandemic. Vaccinating the world also in all of our interests.
What could we learn by comparing a GP to driver in the Grand Prix? Could your surgery be transformed by a Reception Revolution?
Christopher Lowe argues we all need to keep sight of the overall aim of technology: to improve efficiency for both patient and clinician.
Chris Dowrick reviews 'Humanity's conundrum' by David Zigmond. It is easy to become jaded and tired and to lose sight of the therapeutic purpose underlying all of our clinical encounters. Zigmond reminds us to stop, to listen and to respond.
'Perhaps a psychoanalyst would coax out of me that growing my nails is an act of quiet liberation; I can decide how long I want my nails to be, I can decide what I want to next choose for myself. taking control
An experienced GP writes about experiencing bipolar (type 2) disorder, in the hope it will help others to identify and manage the condition.
Martin Hewett argues that because of their understanding of their “duty of care”, doctors make micro-adjustments to their behaviours and work practices to cope with the increased work. This acceptance of the increased workload has two main effects: it sets a new
When you are with a patient and you get a sinking feeling in the pit of your stomach, accompanied by a wish that you were somewhere else, then you are probably facing an ethical problem, writes Peter Toon
Vasumathy Sivarajasingam argues that we need to talk about, and manage, the menopause much better, and reminds us about key aspects that make a huge difference to women's health
Satpal Shekhawat reflects on the problems of an exhausted primary care workforce facing no let-up in workload. Is there a leadership-based solution?
Margaret Jackson and Lesley Morrison argue that GPs should be discussing climate breakdown at every opportunity.
Patients in the UK are able to change the gender marker on their NHS patient record at any time on request, irreversibly removing previous gender identity from their medical record. Does removal of this information pose a challenge to high-quality care for
Peter Toon reflects that removal of mandatory isolation will mean that those who have COVID take on the ethical responsibility for the protection of others. It's complicated...
Primary care clinicians need to be confident business and healthcare management leaders soon after qualification. It's about time this becomes an educational priority to those with the power to shape the educational future of general practice.
Samar Razaq reflects on truth, medical opinion and the scholarship in the age of Twitter.
Matthew Davis and Ana Worthington argue that the arguments in favour of the recent Assisted Dying Bill at its second reading in the UK House of Lords are based on flawed evidence
Helen Burn explains that because legalised physician-assisted dying would likely involve GPs, GPs should think about their views on the issue.
Felicitas Selter, Kirsten Persson, and Gerald Neitzke discuss the similarities and differences in animal and human euthanasia as a source of moral distress for the practitioner.
Andrew Papanikitas, Peter Toon, Paquita De Zulueta, David Misselbrook and John Spicer launch the Ethics of the Ordinary column and reflect on the field of primary care ethics and its relevance
Basem Saab and colleagues from the American University of Beirut illustrate the complexity of COVID-19 requirements and air-travel, for which patients may attend their family doctor for advice and documentation.
Jason Heath, Sangeetha Sornalingam, and Max Cooper highlight the problems the #newnormal is causing to medical education and argue that recognition of this effect is needed before there is lasting damage to the future of the medial profession
What comes to mind when you hear the word bully? Most likely the stereotype of an older child picking on a younger child. But it's important to think of other forms, like the bullying that occurs in our workplaces. Joel Brown explores
As a practising GP, I have come to see myself as a fixer of problems. But does this problem-oriented approach to consultation squander the opportunity we have when we engage our patients in that narrow window? What if we were to re-configure
Louise Hyde argues that we could be doing a lot more to protect children from COVID in the UK