
The morning I wrote this, I read my post. I had received five letters informing me that clients had attended the Emergency Department due to drug overdoses. All of them had been discharged without any intervention. It was remarked in two letters that the clients had reported a sense of hopelessness. This reminded me of so many of my clients who repeatedly overdosed and who, when I emphasised the risk of death with them, told me that they did not care.
The taking of one’s life whether intentionally or through one’s own reckless actions is a tragedy. All victims, young and old, deserve our sympathy. Unfortunately, as a society we do not deal this compassion out equally. There is a hierarchy of empathy that has resulted in an unequal provision of care to those who subsequently die through their own actions. Those who gain most sympathy are the men and women who go on to take their life having had a clear and unambiguous intention to die by their own actions. Usually, they take their own lives as they feel a deep depression and hopeless about their prospects for happiness. This person can come from any background or class. By contrast, those to whom we mete out the least sympathy are those who act recklessly by taking an overdose of drugs, aware that it may result in their loss of life, but not actively seeking to die. Usually, they also feel a deep depression and hopeless about their future prospects for happiness. This person usually comes from a background of poverty and (in the US) is more likely to be black.1 In 2020 there were 5224 deaths in England and Wales due to suicide. This represented a rate of 100 deaths per million of the population.2 In the same year there were 2990 registered poisoning deaths related to drug misuse which represented a rate of 52.3 deaths per million.3
The taking of one’s life whether intentionally or through one’s own reckless actions is a tragedy. All victims, young and old, deserve our sympathy.
So why do we distinguish between these two tragic self-inflicted ways of dying? We distinguish not based on outcome but because of intentionality. Intentionality is of importance to philosophers, particularly ethicists, and lawyers. If a person commits an act, then to determine their moral or legal culpability, it is important to know if they intended to commit that act or not. If they committed the act totally accidentally, then they are ‘innocent’. If they commit the act intentionally, they are ‘guilty’. If they acted recklessly i.e. they knew that their actions may result in the undesired outcome but still acted irrespective of the risk, then they are usually ‘guilty of a lesser crime’. In the middle-ages right up to the late nineteenth century, suicide was viewed through the lens of religion as a sin of such magnitude that often the deceased was denied a burial on church grounds. In this circumstance, it was important to decide whether a person had committed intentional suicide as it had implications for the destination of their corpse and celestial soul. It is still often important from a legal perspective to decide whether someone acted intentionally e.g. in the case of life insurance. In the late nineteenth century, the emphasis shifted from morality. Despite this shift from a moral to a psycho-social understanding of suicide, the concept of intentionality was maintained as a core requirement.
Nowadays, views of suicide are more nuanced – the act is no longer simplistically illegal or immoral. It is a tragedy of unquantifiable proportion, that leaves a devastated family and community behind. And the knowledge that the person was highly depressed and did not envision a future of joy and hope offers little or no relief. However, the loss of someone died recklessly due to an illicit-drug overdose is equally a tragedy leaving devastation behind that is also not relieved by the knowledge of the person experiencing hopelessness.
The question that needs to be asked is whether the concept of intentionality is of relevance to a medical definition of suicide?
The question that needs to be asked is whether the concept of intentionality is of relevance to a medical definition of suicide? What is important for clinicians is to reduce the amount of (predominantly young) people who die because of their own actions. It does not matter if it was done intentionally or recklessly. This is not to say intentionality is not important. It is known that intentionality is a good predictor of completed suicide and so important for assessing suicide risk. However, intentionality to overdose again or suicidal thoughts are also good indicators of risk of a repeat overdose. And there are other indicators of risk that are common to both suicide and illicit-drug overdose such as a previous suicide/overdose attempt, hopelessness, and mood disorders. It has been argued that a history of repeated illicit-drug overdoses, implies an intention to harm or kill oneself or a carelessness about one’s life due to hopelessness.4
The problem is that by focussing on intentionality we have (unintentionally) created a hierarchy around self-inflicted deaths where we pay more attention and provide significantly better healthcare to those higher up this hierarchy.
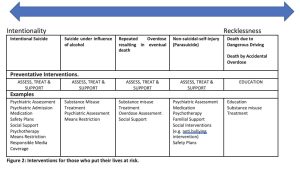
The hierarchy starts at the top with intentional suicide. Taking one’s life when under the influence of alcohol or drugs is down the hierarchy, as it is hard to assess intentionality when capacity is reduced due to alcohol misuse. Non-suicidal-self-injury (NSSI) also known as parasuicide, is further down. NSSI is where there is self-inflicted injury where there is no suicidal intent and for purposes not socially sanctioned. The fundamental differentiating feature between suicide and NSSI is intention to die.4 However, this distinction is muddied by the fact that most patient with NSSI go on to attempt suicide and some die as a result. The long term suicidal risk is between 3-7%.5 Further down the hierarchy, so far down it is not even called suicide, is when people intentionally put their lives at risk by repeatedly overdosing on illicit drugs. At the very end of the spectrum is where people act recklessly (e.g. dangerous driving) knowing it puts their lives at risk. (See Figure 1).
This structural stigma is best described by comparing the healthcare provided to those who have had an attempted suicide due to mood disorder compared to those who have attempted suicide while under the influence of alcohol; those who engage in NSSI; and those who have had multiple non-fatal illicit-drug over-doses.
If you attempt suicide, you will automatically receive a psychiatric assessment. If you are judged to be at risk of a repeat attempt, you will be admitted to a psychiatric unit to ensure your safety. If you have repeated suicide attempts, the likelihood is you will be admitted.
If you attempt suicide while under the influence of alcohol, you will automatically receive a psychiatric assessment. However, the assessing doctor will wait for you to sober up as alcohol is presumed to affect your capacity to make intentional decisions. Yet as Klimkiewicz et al (2012) suggest, if one is focussing on prevention of death, it may be inappropriate to evaluate intentionality when sober, as most suicide attempts inebriated are unplanned. An evaluation of the risk of relapse onto alcohol may be a better indicator.6 We know that that clients with alcohol misuse disorder are up to 4.6 times more likely to die by suicide when intoxicated than when sober.6 It has been claimed that risk factors for suicide under the influence of alcohol are under researched in comparison to those for sober suicide.
Patients who engage in NSSI will receive an assessment. However, they are often subject to stigmatising attitudes from health professionals. This stigma has been shown to cloud physicians’ judgment, reduce their compassion, on occasions result in punitive behaviours and to result in poor outcomes (e.g. clients self-discharging from emergency departments before completion of assessment or clients doing further self-injury as a result of feelings arising from the lack of compassion). This stigma exists despite the known higher rate of completed suicide in this population.7
If you have a non-fatal illicit-drug overdose, you will not receive an automatic assessment. This is even though we have interventions that are known to reduce the risk of subsequent overdose. If you are judged to be at risk of a repeat overdose, you will not be admitted to a place of safety. It is known that people who use drugs (PWUD) are subject to significantly worse stigma than almost any other stigmatised group (including people with a mood disorder) and that this experience of stigma increases the risk of a fatal and non-fatal overdose. It is further known that healthcare workers often display this societal stigma, often believing PWUD to be at fault for their own lifestyle and that this stigma often results in poorer healthcare for PWUD.
This is not to argue either for or against the suggestion that PWUD who overdose frequently should be compulsorily admitted to a place of safety. It is to point out the disparity in attention and safeguarding we offer those who attempt suicide compared to those who overdose. If we were to address this disparity we would provide appropriate assessment, support and treatment for those who do not fit the present definition for suicide.(See Fig 2)
In summary, we have over relied on a legalistic/moralistic definition of suicide that serves us poorly in present day medicine. We should group these deaths under self-inflicted deaths of despair. Then we could identify the varying risk factors for those who put their lives at risk due to their own actions and come up with an appropriate clinical and social response to help prevent them putting their lives at risk again. This could offer a more clinically effective response and a more humane and less stigmatising one as well.
References
1. Emyr John, Asim Butt Deaths related to drug poisoning in England and Wales: 2019 registrations Deaths related to drug poisoning in England and Wales from 1993 to 2019, by cause of death, sex, age and substances involved in the death. Office for National Statistics Statistical Bulletin 2020
2. https://researchbriefings.files.parliament.uk/documents/CBP-8221/CBP-8221.pdf
3. Deaths related to drug poisoning in England and Wales: 2020 registrations. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/2020
4. Halicka J, Kiejna A. Non-suicidal self-injury (NSSI) and suicidal: Criteria differentiation. Adv Clin Exp Med. 2018 Feb;27(2):257-261. doi: 10.17219/acem/66353. PMID: 29521070.
5. Soomro GM, Kakhi S. Deliberate self-harm (and attempted suicide). BMJ Clin Evid. 2015 May 28;2015:1012. PMID: 26032238; PMCID: PMC4451502
6. Klimkiewicz A, Ilgen MA, Bohnert AS, Jakubczyk A, Wojnar M, Brower KJ. Suicide attempts during heavy drinking episodes among individuals entering alcohol treatment in Warsaw, Poland. Alcohol Alcohol. 2012 Sep-Oct;47(5):571-6. doi: 10.1093/alcalc/ags069. Epub 2012 Jun 12. PMID: 22691386; PMCID: PMC3500855.
7. Tapola V, Wahlström J, Lappalainen R. Effects of training on attitudes of psychiatric personnel towards patients who self-injure. Nurs Open. 2016 Feb 17;3(3):140-151. doi: 10.1002/nop2.45. PMID: 27708824; PMCID: PMC5047340.
Featured image: Photo by Dan Meyers on Unsplash









16
Today on International Overdose Awareness Day, Correlation wants to reflect on the current situation regarding overdose, overdose prevention, and non-fatal overdose in Europe.
C-EHRN reached out to our focal points for their insight into the current overdose situation in Europe.
Following the data from our 2021 Data Report, we can see that the life-saving drug Naloxone is still not widely available. Naloxone can reverse the effects of an overdose, and consequently save lives; our advocacy work pushes for the availability of naloxone worldwide. Karen Mamo from our focal point in Malta offered the below reflection on Naloxone;
Tony Duffin of Ana Liffey, our Irish focal point, offered the below sentiment regarding non-fatal overdose;
Dr Austin O’Carroll was inspired by his work with people who use drugs, and offered the below reflection on overdose;
The full paper from Dr Austin O Carroll is available here.
In Greece, the rising mortality rates of people who use drugs continue to rise, with a large HIV outbreak among people who inject drugs (PWID) in Athens, Greece. A paper regarding these worrying rates can be accessed here.
Marios Atzemis, of Positive Voice, offered a concerning insight into the situation in Greece;
In the coming weeks, more research regarding the concerning rise in mortality rates in Greece will be shared within the network to raise awareness of the situation and to support advocacy work for this problem. Both Marios Atzemis and Christos Siou will take part in a conversation with C-EHRN regarding this issue, which will be shared within the network to further support advocacy and awareness.
Earlier this year, C-EHRN hosted a webinar on the state and challenges of overdose prevention, the webinar recording can be accessed here. Read our monitoring report with information on overdose here.
Visit the official International Overdose Awareness Day site here.