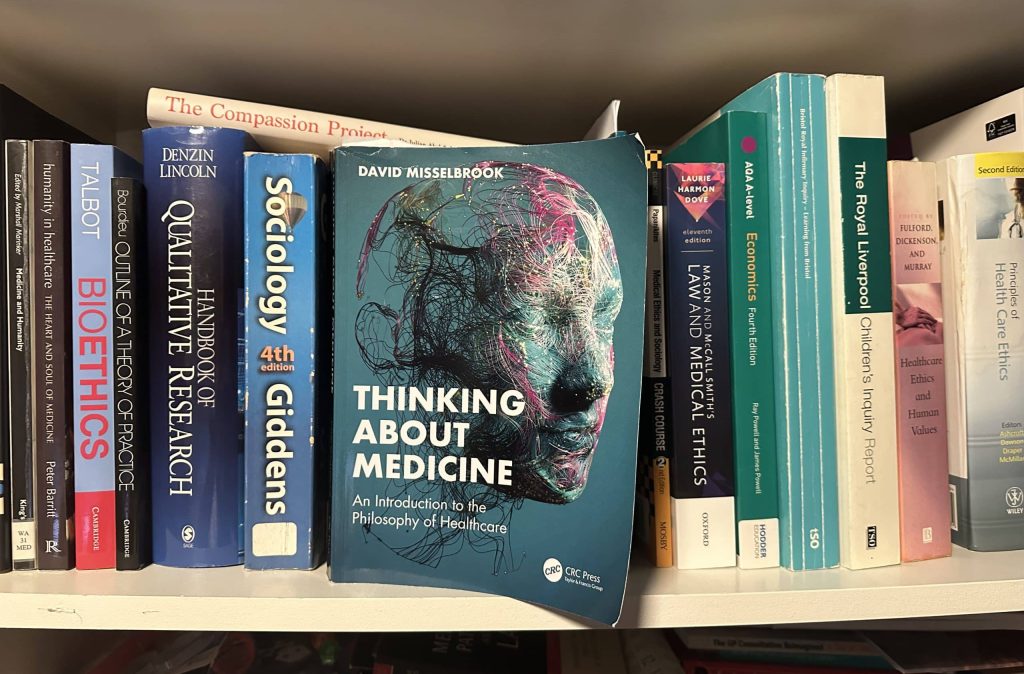
Misselbrook masterfully uses the tools of philosophy to explain to us how we think the way we do, how we can think more clearly. In a political climate dominated by polarising and often poisonous rhetoric, bullshit-detection skills are the least of what
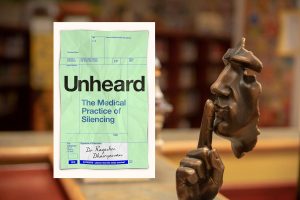
The practice of silencing is unjust and unfair, but probably universal in medicine. Trisha Greenhalgh reflects on a 'powerful' new book that is packed with compelling patient stories and accessible summaries of the academic literature. And for the teachers and trainers among
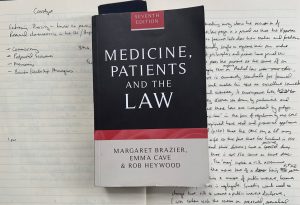
Andrew Papanikitas reviews and reflects on a good critical sourcebook on the law for GP trainers and trainees looking to flesh out a case-based discussion or tutorial, as well as for the GP looking for reading in response to a patient unmet
Kindness is a disposition that can’t be policed and which grows out of care, attention and connection. To suggest it can be enforced and regulated for is a mistake, explain Rupal Shah and colleagues.
What are 'Ordinary' worries? Elke Hausmann reflects in the light of recent announcements by the prime minister about taking sick note prescribing away from GPs, with the argument that 'normal worries' are being wrongly medicalised as mental illness, also using that to
To be fit for work, a person must be capable of more than simply carrying out in isolation the tasks required by their role: they must be able to do so repeatedly, to a consistent standard, and in a way that represents
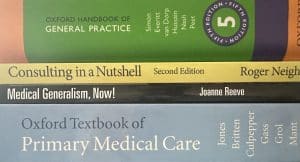
Establishing general practice first as an independent subject or specialism, and then as a university discipline has been a major challenge over many decades. Where we are at present doesn’t appear to be working. Howie, Freeman, and heath reflect on what we
...an apparent paradox makes science possible. At least two conditions are necessary, and they appear deeply contradictory. The first is that the universe must be governed by consistent physical laws, the second is that humans in general, and scientists in particular, must
Richard Armitage's reading about Chalmers’ proposal of two distinct Problems (the capital is deliberate) of consciousness sparked an analogy in the domain of human health...
There has been significant debate recently around how best to name the newest healthcare profession to seek regulation under the umbrella of the Professional Standards Authority (PSA). Cathal Gallagher reflects on the legality of the title 'Doctor'.
The author strongly supports a woman’s right to choose, arguing for the decriminalisation of abortion in the UK, suggesting that it should be regulated as a part of healthcare. She describes recent cases where women have been given custodial sentences which have
Investigations themselves can throw up results that are difficult to interpret, and they may reveal abnormalities of uncertain significance. To highlight these issues to our patients would constitute more ethical practice, would foster greater patient empowerment, and could result in a frame
Notwithstanding the corny connection to a fictional character, and the 'old school' approach to confidentiality, this is a charming and authentic memoir. An anecdote is by definition an unpublished story - and Martin Stagg has converted his anecdotes into 'ecdotes.'
Alex Burrell reflects on the moral agonies of planning an early GP-career
The Lancet declares that “generative AI is not an author”, and dictates that “these tools should only be used to improve language and readability”. But are these statements – the first a factual claim, the second a normative assertion – entirely true?
...requests for race-based concordance is a complicated area of medicine, and it is one that is not easily dealt with through formulised policies. Instead, well-reasoned judgements by the care team through a deliberative process, that begin with ethical frameworks, might provide a
Esoteric morality refers to the idea that it might sometimes be right to do or recommend privately actions that it would be wrong to advocate openly, if doing so secretly would have better overall consequences. Richard Armitage asks what this might mean
In this provocative essay, Richard Armitage explores what a respect for autonomy requires of GPs, its manifestation as the patient’s ‘right’ not to know, and the problems this raises for contemporary general practice.
David Jeffrey argues that clinical curiosity is an essential part of a doctor’s empathy and clinical decision-making. It promotes reflective practice, critical thinking and stimulates lifelong learning.
Carter Singh argues that accusing striking doctors of causing harm is disingenuous when there are many critical harms that strikes are attempting to address.
So, how can GPs help their patients in facing transformative decisions? The advice, helpfully explained by Richard Armitage, is to reframe the decision-making process with which we approach them.
Variety is a selling point for the profession itself (challenging and interesting) and for the resources needed to do it well (GPs are ‘best’ placed to do many great things but need time and money invested). Andrew Papanikitas introduces this month's Life
Richard Armitage argues that, in three well-defined contexts, clinical decision-making should be delegated to AI systems either today or in the very near future.
GPs allow patients to make harmful choices – thereby affording primacy to autonomy at the expense of beneficence – when that harm accrues only to the individual making such choices. But if your future self is a different person, does that mean
'When reading the spread of articles in this issue it struck me that we need diversity to be better clinicians, colleagues, and citizens.' Andrew Papanikitas reflects this month's Life and Times articles, discussing gender, diversity, narrative and queer bioethics.
It is a brief and easily searchable quick reference. and it covers key ethical tools to think through a case and it covers key aspects of the law as well as a variety of practice specific situations, but has an interesting flaw...
Slight changes in phraseology can dramatically alter the central meaning of a vitally important principle. By “consenting the patient” instead of “seeking meaningful consent,” the right of our patients to be involved in choices about their treatment and care... is exchanged with
In 'Would you kill the fat man?' Edmonds takes a well-known philosophical thought experiment – commonly known as the ‘trolley problem,’ and explores it and its various iterations in a fun, fresh, stimulating read.
Crowdfunding of direct medical costs raises some ethical issues which may legitimately concern health professionals and should concern regulators. Kathryn Millard explores the key issues.
Foell and colleagues argue that assembly-line approaches in manufacturing rely on accurately measuring the time it takes to perform tasks in a digitalised workplace. They juxtapose this with the concept of time as the time it takes in the mystery of General
Richard Armitage highlights a selection of issues in tension with public health and respiratory communicable diseases both pre and post the outbreak of COVID-19.
Assessing the effectiveness of each charitable project and directing financial donations to the one that ranks highest is certainly a task of gargantuan proportions. Richard Armitage explains.
While various definitions of health have been offered over recent centuries, the search for an enduring and completely satisfying definition has proven frustratingly elusive. Richard Armitage wrestles with one of the most recent and promising definitions.
The clocks going back as we descend into winter each year generates an additional hour that we generally choose to spend asleep. A poignant philosophical reflection on time.
You need to keep going, but stray too far to the left and you’ll be over the cliff edge before you know it; go too far to the right and you’ll be bogged down, and who knows what state you’ll be in
Due to the accelerating power of our technological arsenal, and the contrasting stasis of our professional wisdom, the intelligence-wisdom gap is expanding at a blistering pace. With formidable technologies on the scientific horizon – nanotechnology, CRISPR, and general-purpose AI – the necessity
Should healthcare professionals ever strike? For some healthcare professionals, going on strike crosses a professional and moral line. Nada Khan explores the debate.
Tom Brett had known Martha as a patient for fifteen years. Widowed for over 25 years, she had moved from the family farm to settle in the city close to her children...
Richard Armitage suggests it is right for GPs to primarily regard their beneficiaries as ‘agents’ rather than ‘patients’ in the majority of general practice consultations.
Increased dialogue about the unique nuances of physicians adopting the role of ‘patient’ should be supported throughout medical training, argues Isabella de Vere Hunt.