Alex Burrell is a GP in Bristol.
Alex Burrell is a GP in Bristol.
Yonder is a diverse selection of primary care relevant research stories from beyond the mainstream biomedical literature.
Improving connections
In 2018, the Welsh Government set out a national Transformation Programme committing targeted funding to new models of partnership between health, social care, and third sector organisations. One such model in the Cardiff South West Primary Care Cluster – made up of 11 GP practices serving 74 000 people — aimed to reduce emergency admissions through developing multidisciplinary working and focusing on ‘improved connections between patients and communities, and across services’.1 Four key elements were implemented: a bi- weekly community multidisciplinary team meeting including GPs; a discharge liaison hub to identify and contact potentially vulnerable patients following hospital discharge; community wellbeing connectors (social prescribers); and advance care planning training and recording. It’s well worth reading the full article to go through all the outcomes reported (though this is not a formal evaluation), but two things stand out. First, the primary aim was met with a reduction in admissions and hospital bed days with corresponding cost savings. Second, the quotes from GPs involved are heartening: ‘it’s what I thought general practice would be about when I started, which was looking at people holistically … this has totally rejuvenated my experience of general practice’.
AI in reflective practice
Reflective practice is a fundamental component of GP training and post-CCT life, with ongoing requirements for professional development, appraisal, and revalidation. While self- reflection may come naturally to some, for others it can be a painstaking process. The authors of this article suggest that AI, and in particular large language models (LLMs) such as ChatGPT, may have potential to develop and improve reflective practice through ‘refram[ing] experiences and foster[ing] deeper self- reflection’.2 They used three case vignettes, composites with elements of real scenarios and no patient identifiable information, entered into ChatGPT with different prompts given. For example, a structured reflection with a GP registrar in mind asks the LLM to take the user through the stages of the Gibbs reflective cycle one question at a time. Or, for a more experienced GP, to go through a difficult case using reflective questions inspired by Brian Eno’s Oblique Strategy cards. The questions generated by challenging cases are insightful and require deep reflection and self- examination. The authors carefully consider the ethical and practical challenges, in particular privacy and data security, but there is clearly potential here.
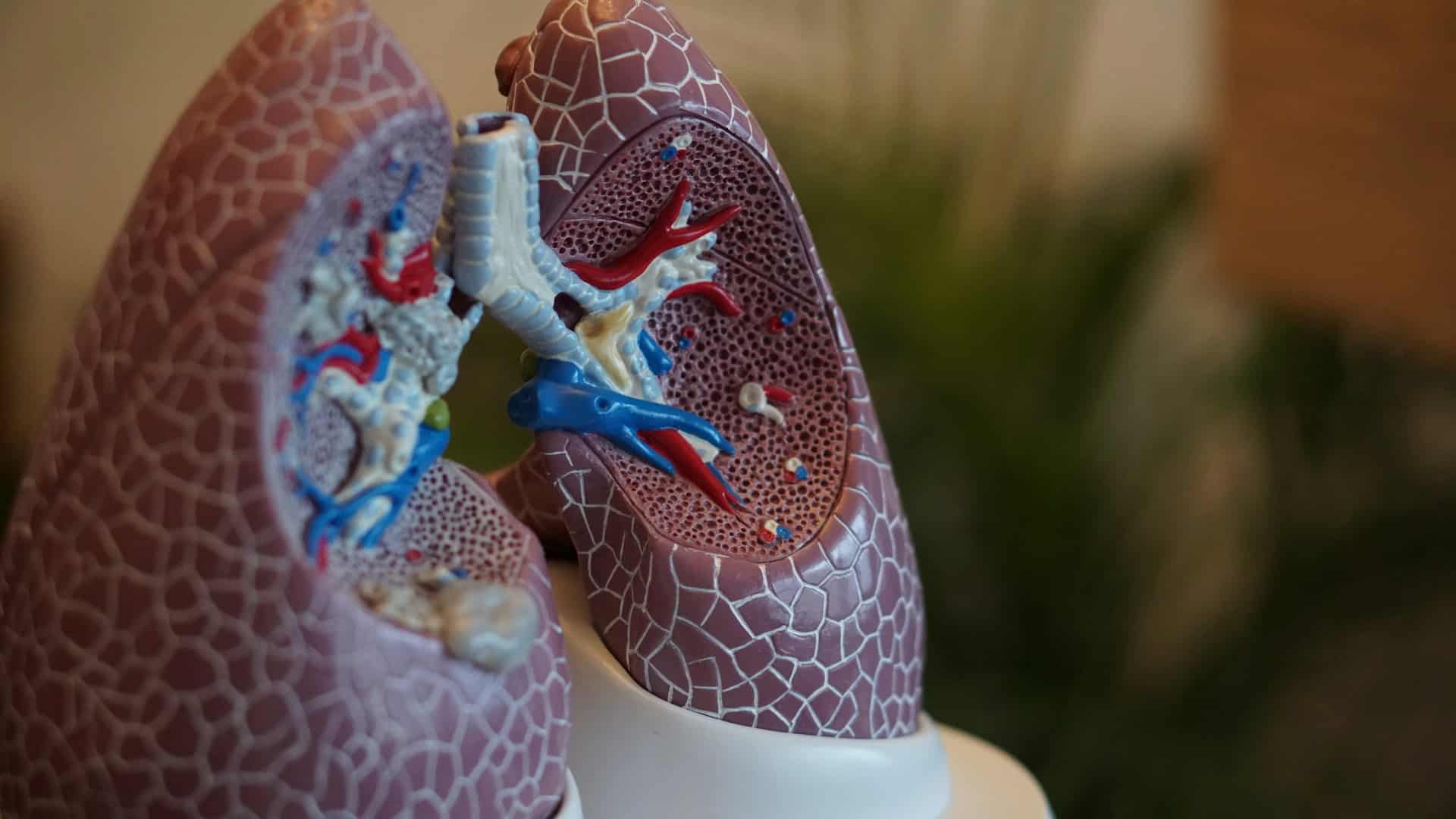
Lung cancer diagnosis
Lung cancer survival rates in the UK are relatively poor compared to other high- income countries, at least in part due to later stage at diagnosis. Shortening the diagnostic interval (DI), the time between first presentation to primary care with potential cancer symptoms and cancer diagnosis, could improve things: lung cancer has a particularly high number of pre-referral consultations, which the authors of this large database study suggest could be due to the presence of comorbid conditions.3 In total, 11 870 patients with lung cancer were included in the final analysis, which showed that patients with ≥1 condition/s that offered an alternative explanation for lung cancer symptoms, for example, chronic obstructive pulmonary disease or asthma, had significantly increased DI compared to those without: 31 days for one condition, 74 days for two or more. Conditions that only presented competing demands, for example, unrelated to lung cancer symptoms but placing a demand on physicians’ time and drawing focus, were not found to contribute significantly to DI. The authors suggest this reminder of the difficulty of diagnosing lung cancer in the presence of comorbidities supports proposals for lung cancer screening programmes for earlier detection.
Euthanasia aftercare
Euthanasia, or physician-assisted suicide (EAS), has been legal in the Netherlands since 2002 under strict legal criteria and approximately 9000 people underwent EAS there in 2021. In the absence of clear guidelines on bereavement support following EAS, this questionnaire study surveyed 127 physicians working in adult medicine, mostly GPs, on their experience of EAS and bereavement support.4 GPs were more likely to have had an aftercare conversation than specialists (82.2% versus 53.8%), and physicians reported three main topics in aftercare conversations: looking back on the practical aspects of EAS; the emotional experiences of relatives during the EAS process; and the mental wellbeing of relatives following EAS. There is scope for far more in-depth exploration of bereavement in these circumstances, but this does introduce an important topic for consideration in the ongoing debate on EAS in the UK.
References
1. Withers K, Pardy K, Topham L, et al. A long way from Frome: improving connections between patients, local services and communities to reduce emergency admissions. BMC Prim Care 2024; 25(1): 307.
2. Lewis M, Hayhoe B. The digital Balint: using AI in reflective practice. Educ Prim Care 2024; DOI: 10.1080/14739879.2024.2372606.
3. Rogers I, Cooper M, Memon A, et al. The effect of comorbidities on diagnostic interval for lung cancer in England: a cohort study using electronic health record data. Br J Cancer 2024; 131(7): 1147–1157.
4. Renckens SC, Pasman HR, van der Heide A, Onwuteaka-Philipsen BD. Aftercare provision for bereaved relatives following euthanasia or physician-assisted suicide: a cross-sectional questionnaire study among physicians. Int J Public Health 2024; 69: 1607346.
Featured photo by Robina Weermeijer on Unsplash.