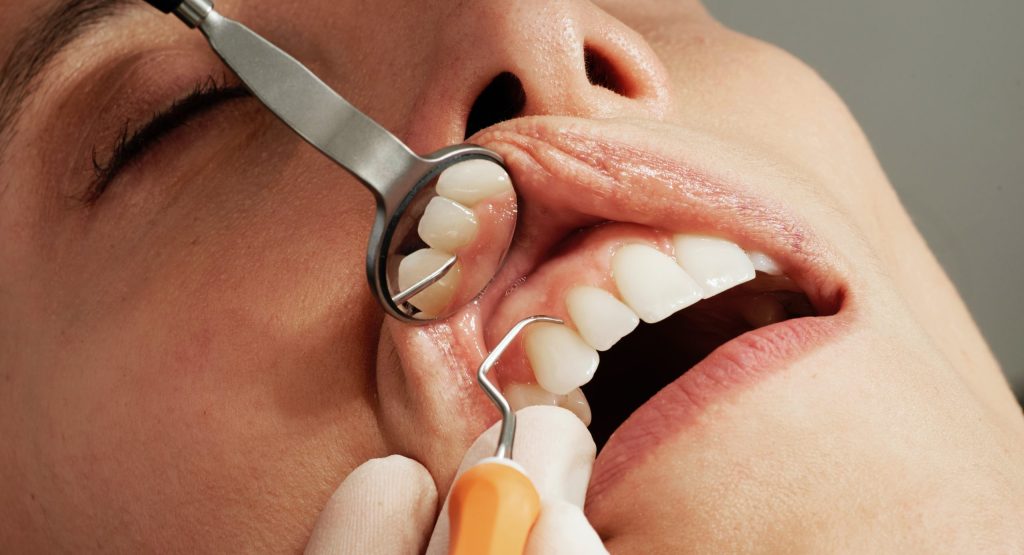
Why face-to-face still saves lives
Remote consulting is excellent for repeat prescriptions, routine results, straightforward infections in the young and well, and selected mental health follow-ups. But general practice is not primarily populated by the young and well..