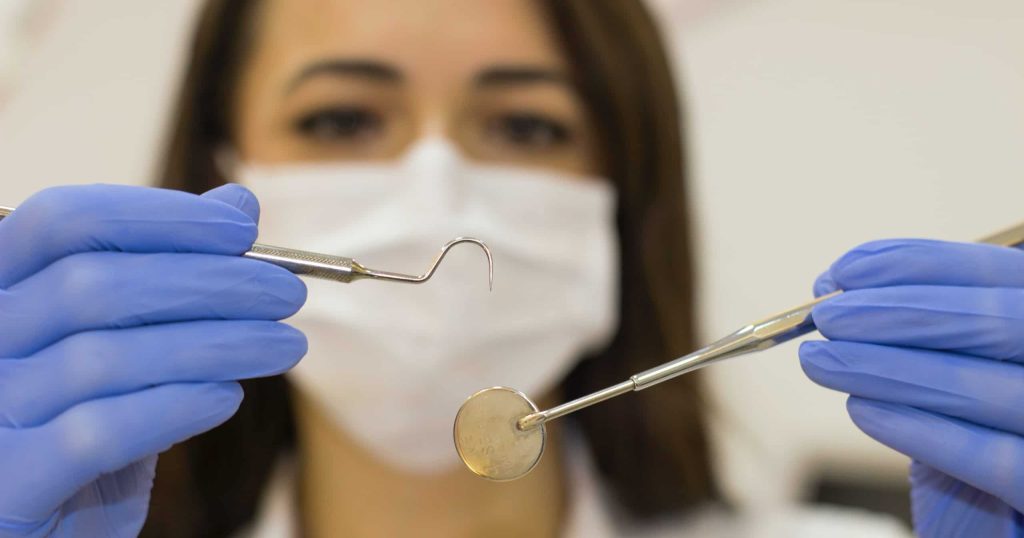
Undervalued and unsustainable: The economic reality of GP minor surgery services
When the price of a portion of fish and chips has tripled in 20 years but the tariff for a joint injection remains static, something has gone seriously wrong with how we value general practice.